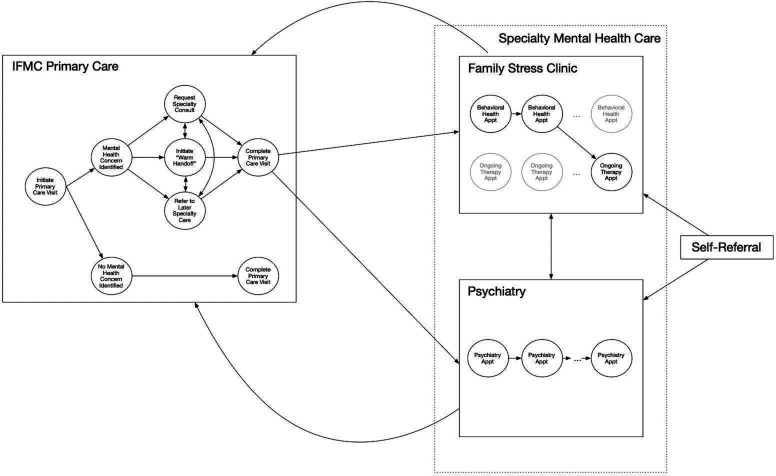
Integrated model of primary and mental healthcare for the refugee population served by an academic medical centre.
IF 4.3
3区 医学
Q1 PRIMARY HEALTH CARE
引用次数: 0
Abstract
Refugees are at increased risk for developing mental health concerns due to high rates of trauma exposure and postmigration stressors. Moreover, barriers to accessing mental health services result in ongoing suffering within this population. Integrated care—which combines primary healthcare and mental healthcare into one cohesive, collaborative setting—may improve refugees’ access to comprehensive physical and mental health services to ultimately better support this uniquely vulnerable population. Although integrated care models can increase access to care by colocating multidisciplinary services, establishing an effective integrated care model brings unique logistic (eg, managing office space, delineating roles between multiple providers, establishing open communication practices between specialty roles) and financial (eg, coordinating across department-specific billing procedures) challenges. We therefore describe the model of integrated primary and mental healthcare used in the International Family Medicine Clinic at the University of Virginia, which includes family medicine providers, behavioural health specialists and psychiatrists. Further, based on our 20-year history of providing these integrated services to refugees within an academic medical centre, we offer potential solutions for addressing common challenges (eg, granting specialty providers necessary privileges to access visit notes entered by other specialty providers, creating a culture where communication between providers is the norm, establishing a standard that all providers ought to be CC’ed on most visit notes). We hope that our model and the lessons we have learned along the way can help other institutions that are interested in developing similar integrated care systems to support refugees’ mental and physical health.
由学术医疗中心为难民人口提供初级和精神保健的综合模式。
由于创伤暴露率高和移民后压力因素,难民出现心理健康问题的风险增加。此外,获得精神卫生服务的障碍导致这一人群持续遭受痛苦。综合护理——将初级保健和精神保健结合到一个有凝聚力的协作环境中——可能会改善难民获得全面身心健康服务的机会,最终更好地支持这一独特的弱势群体。虽然综合护理模式可以通过整合多学科服务来增加获得护理的机会,但建立一个有效的综合护理模式带来了独特的后勤(例如,管理办公空间,描述多个提供者之间的角色,在专业角色之间建立开放的沟通实践)和财务(例如,协调跨部门特定的计费程序)挑战。因此,我们描述了弗吉尼亚大学国际家庭医学诊所使用的综合初级和精神保健模式,其中包括家庭医学提供者、行为健康专家和精神科医生。此外,根据我们在学术医疗中心向难民提供这些综合服务的20年历史,我们为解决共同挑战提供了潜在的解决方案(例如,授予专业提供者访问其他专业提供者输入的就诊记录的必要特权,创造一种提供者之间沟通成为常态的文化,建立一种标准,所有提供者都应该抄送大多数就诊记录)。我们希望我们的模式和我们在此过程中所学到的经验教训可以帮助其他有兴趣开发类似综合护理系统的机构,以支持难民的身心健康。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Family Medicine and Community Health
PRIMARY HEALTH CARE-
CiteScore
9.70
自引率
0.00%
发文量
27
审稿时长
19 weeks
期刊介绍:
Family Medicine and Community Health (FMCH) is a peer-reviewed, open-access journal focusing on the topics of family medicine, general practice and community health. FMCH strives to be a leading international journal that promotes ‘Health Care for All’ through disseminating novel knowledge and best practices in primary care, family medicine, and community health. FMCH publishes original research, review, methodology, commentary, reflection, and case-study from the lens of population health. FMCH’s Asian Focus section features reports of family medicine development in the Asia-pacific region. FMCH aims to be an exemplary forum for the timely communication of medical knowledge and skills with the goal of promoting improved health care through the practice of family and community-based medicine globally. FMCH aims to serve a diverse audience including researchers, educators, policymakers and leaders of family medicine and community health. We also aim to provide content relevant for researchers working on population health, epidemiology, public policy, disease control and management, preventative medicine and disease burden. FMCH does not impose any article processing charges (APC) or submission charges.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


