Incidence of Acute Kidney Injury and Risk Factors of Prognosis in Patients with Acute Stanford Type A Aortic Dissection.
IF 1.3
4区 医学
Q4 CARDIAC & CARDIOVASCULAR SYSTEMS
Annals of Thoracic and Cardiovascular Surgery
Pub Date : 2023-10-20
Epub Date: 2023-04-01
DOI:10.5761/atcs.oa.22-00242
引用次数: 0
Abstract
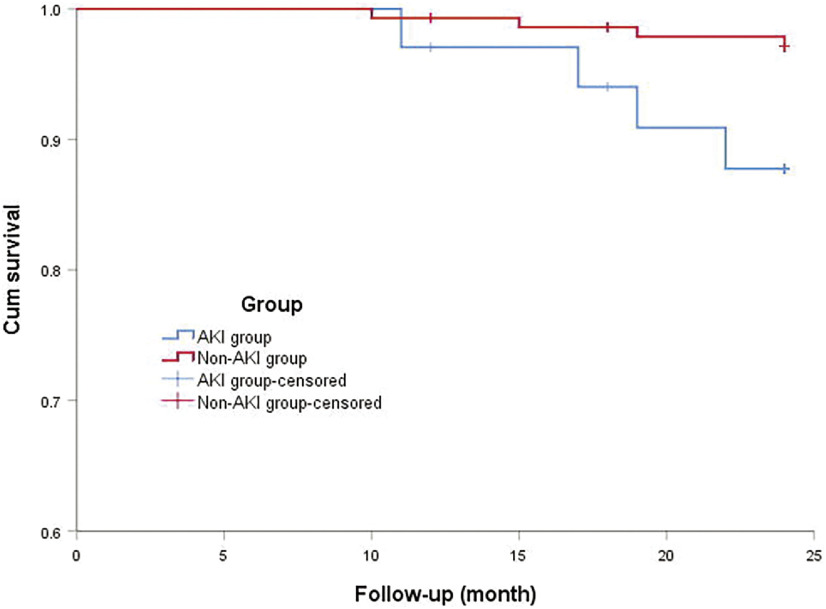
Purpose: We aimed to investigate the prognosis and impact of postoperative acute kidney injury (AKI) in acute Stanford type A aortic dissection (ATAAD) patients, and to analyze the predictors of short- and medium-term survival. Methods: A total of 192 patients who underwent ATAAD surgery were included between May 2014 and May 2019. Perioperative data of these patients were analyzed. All of the discharged patients were followed up for 2 years. Results: Postoperative AKI was identified in 43 of 192 patients (22.4%). The two-year survival rate of patients with AKI after discharge was 88.2% and that without AKI was 97.2%.The difference was statistically significant (χ2 = 5.355, log-rank P = 0.021). Cox hazards regression showed that age (hazard ratio [HR], 1.070; P = 0.002), cardiopulmonary bypass (CPB) time (HR, 1.026; P = 0.026), postoperative AKI (HR, 3.681; P = 0.003), and red blood cell transfusion (HR, 1.548; P = 0.001) were independent risk factors for the short- and medium-term total mortality of ATAAD patients. Conclusion: The incidence of postoperative AKI is high in ATAAD, and the mortality of patients with AKI increases significantly within 2 years. Age, CPB time, and red blood cell transfusion were also independent risk factors for short-and medium-term prognoses.
急性斯坦福A型主动脉夹层患者的急性肾损伤发生率和预后危险因素。
目的:我们旨在研究急性斯坦福A型主动脉夹层(ATAAD)患者术后急性肾损伤(AKI)的预后和影响,并分析短期和中期生存率的预测因素。方法:纳入2014年5月至2019年5月期间接受ATAAD手术的192名患者。对这些患者的围手术期数据进行分析。所有出院患者均进行了2年的随访。结果:192例患者中43例(22.4%)发现术后AKI。有AKI的患者出院后2年生存率为88.2%,无AKI的为97.2%。差异有统计学意义(χ2=5.355,log秩P=0.021)。Cox危险因素回归显示年龄(危险比[HR],1.070;P=0.002)、体外循环(CPB)时间(HR,1.026;P=0.026),术后AKI(HR,3.681;P=0.003)和红细胞输注(HR,1.548;P=0.001)是ATAAD患者中短期总死亡率的独立危险因素。结论:ATAAD患者术后AKI发生率高,2年内AKI患者死亡率显著升高。年龄、体外循环时间和红细胞输注也是中短期预后的独立危险因素。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Annals of Thoracic and Cardiovascular Surgery
CARDIAC & CARDIOVASCULAR SYSTEMS-SURGERY
CiteScore
2.80
自引率
0.00%
发文量
56
审稿时长
4-8 weeks
期刊介绍:
Information not localized
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


