Computational design of custom therapeutic cells to correct failing human cardiomyocytes.
IF 2.3
引用次数: 0
Abstract
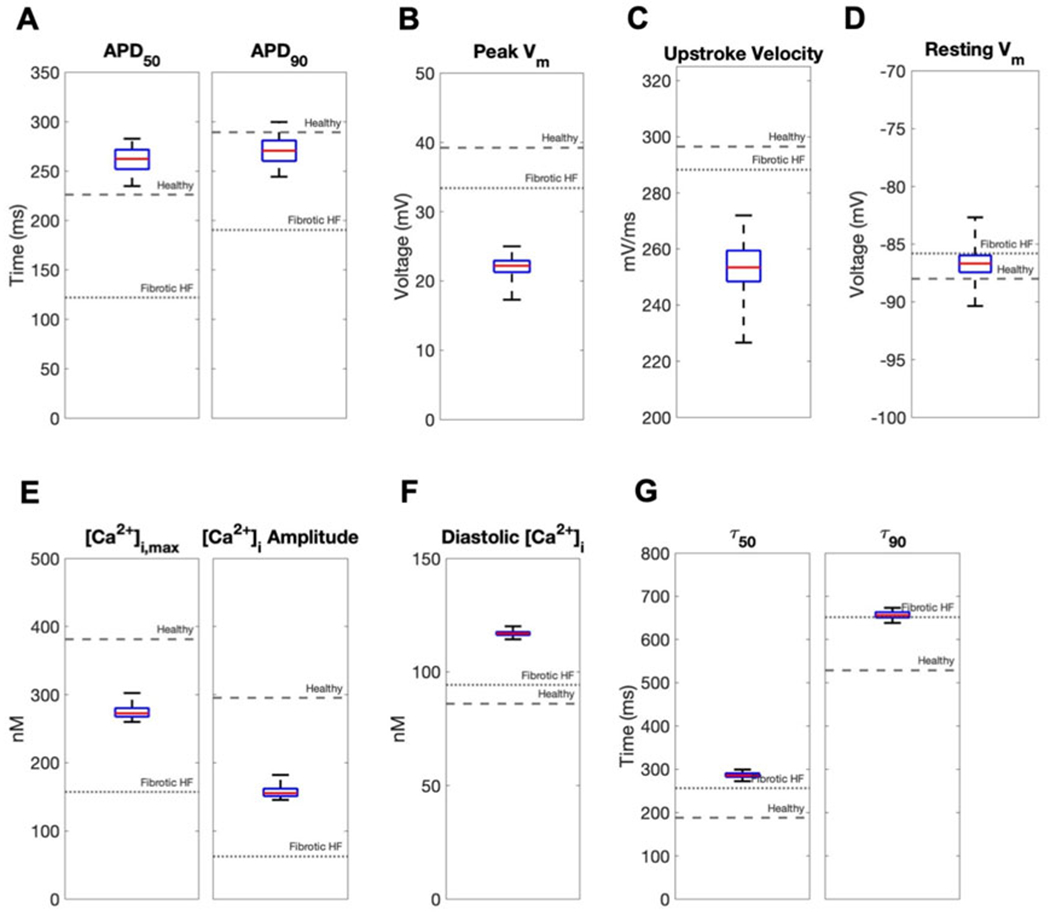
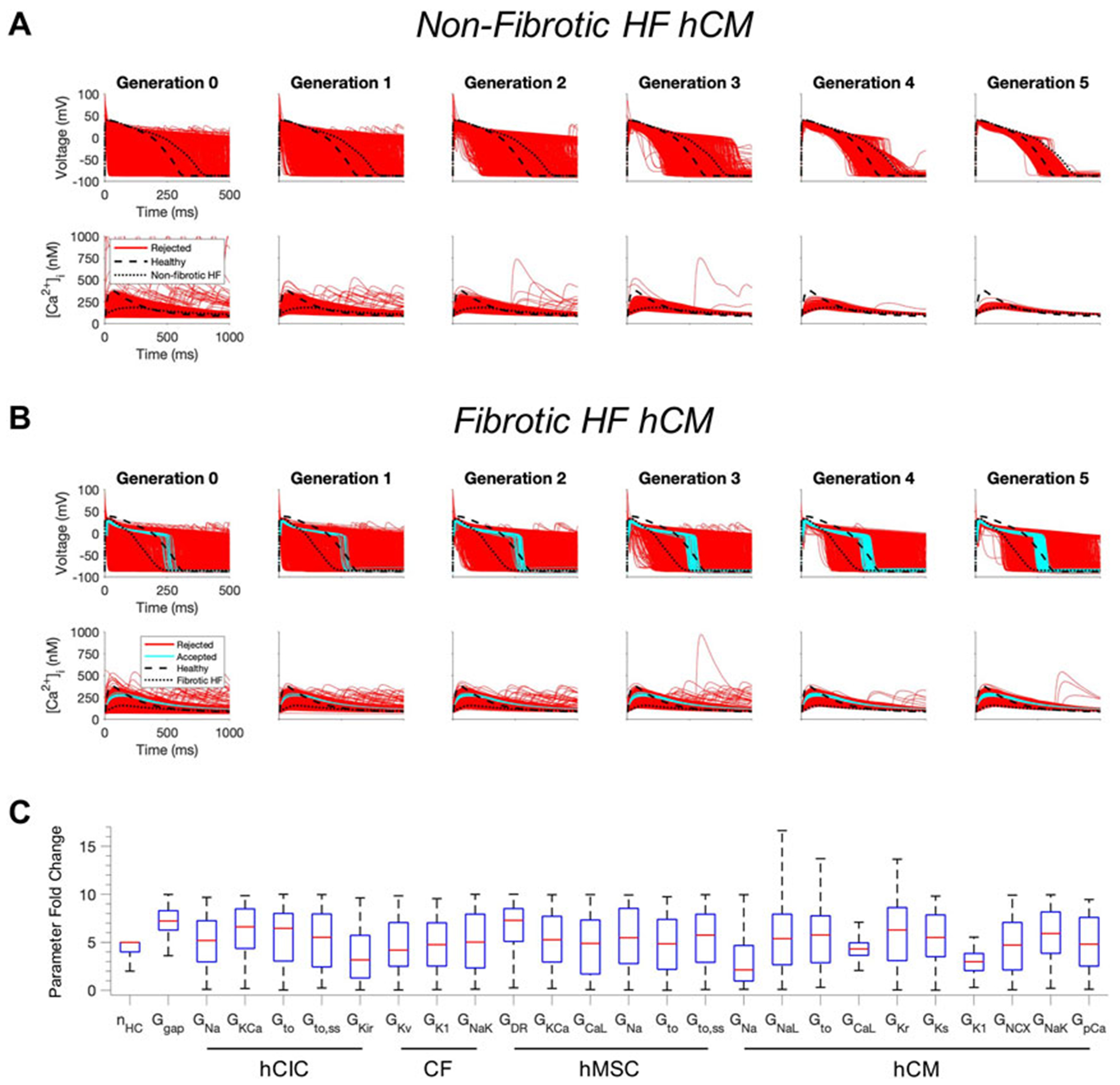
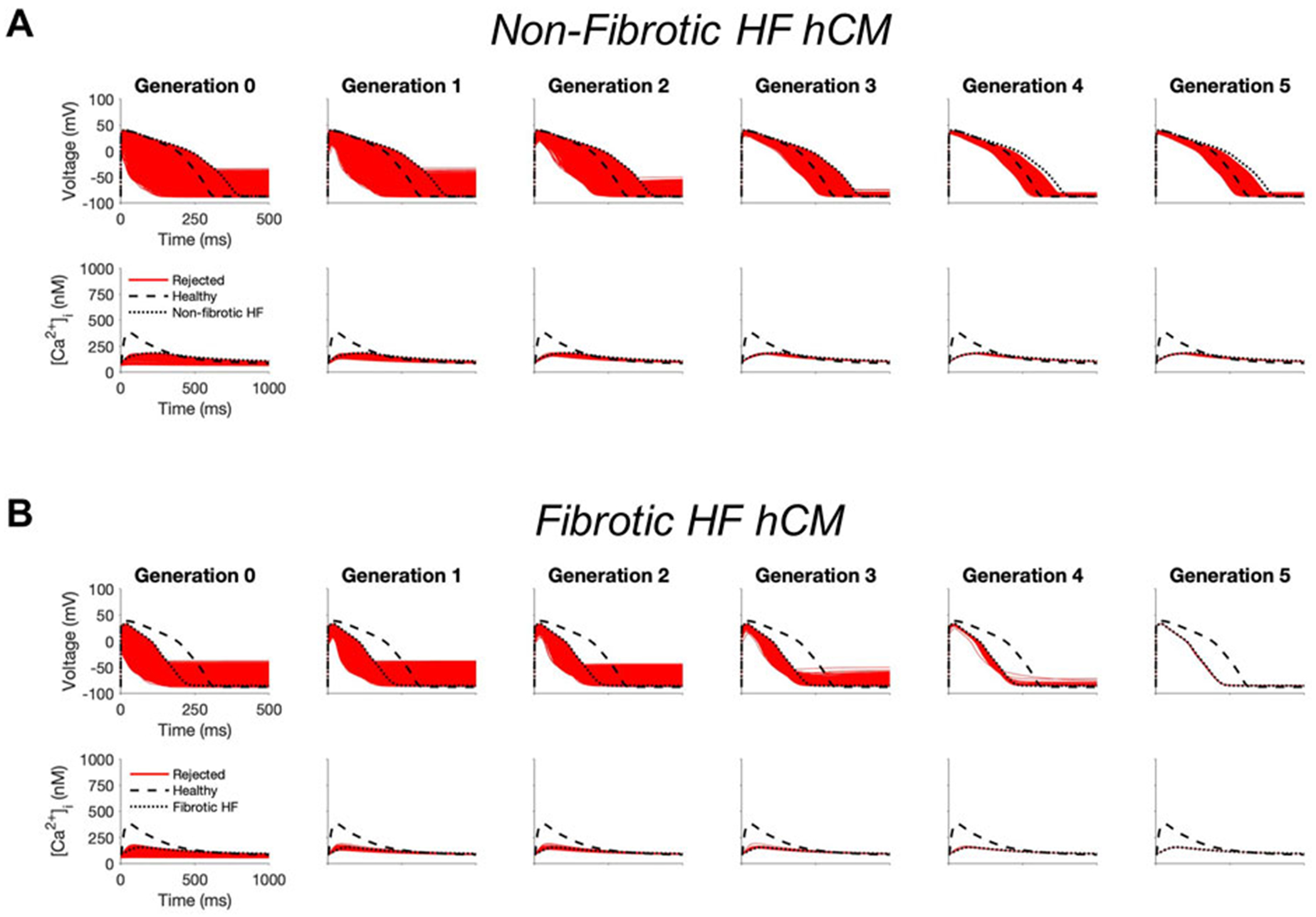
Background: Myocardial delivery of non-excitable cells—namely human mesenchymal stem cells (hMSCs) and c-kit+ cardiac interstitial cells (hCICs)—remains a promising approach for treating the failing heart. Recent empirical studies attempt to improve such therapies by genetically engineering cells to express specific ion channels, or by creating hybrid cells with combined channel expression. This study uses a computational modeling approach to test the hypothesis that custom hypothetical cells can be rationally designed to restore a healthy phenotype when coupled to human heart failure (HF) cardiomyocytes. Methods: Candidate custom cells were simulated with a combination of ion channels from non-excitable cells and healthy human cardiomyocytes (hCMs). Using a genetic algorithm-based optimization approach, candidate cells were accepted if a root mean square error (RMSE) of less than 50% relative to healthy hCM was achieved for both action potential and calcium transient waveforms for the cell-treated HF cardiomyocyte, normalized to the untreated HF cardiomyocyte. Results: Custom cells expressing only non-excitable ion channels were inadequate to restore a healthy cardiac phenotype when coupled to either fibrotic or non-fibrotic HF cardiomyocytes. In contrast, custom cells also expressing cardiac ion channels led to acceptable restoration of a healthy cardiomyocyte phenotype when coupled to fibrotic, but not non-fibrotic, HF cardiomyocytes. Incorporating the cardiomyocyte inward rectifier K+ channel was critical to accomplishing this phenotypic rescue while also improving single-cell action potential metrics associated with arrhythmias, namely resting membrane potential and action potential duration. The computational approach also provided insight into the rescue mechanisms, whereby heterocellular coupling enhanced cardiomyocyte L-type calcium current and promoted calcium-induced calcium release. Finally, as a therapeutically translatable strategy, we simulated delivery of hMSCs and hCICs genetically engineered to express the cardiomyocyte inward rectifier K+ channel, which decreased action potential and calcium transient RMSEs by at least 24% relative to control hMSCs and hCICs, with more favorable single-cell arrhythmia metrics. Conclusion: Computational modeling facilitates exploration of customizable engineered cell therapies. Optimized cells expressing cardiac ion channels restored healthy action potential and calcium handling phenotypes in fibrotic HF cardiomyocytes and improved single-cell arrhythmia metrics, warranting further experimental validation studies of the proposed custom therapeutic cells.
定制治疗细胞的计算设计,以纠正失败的人类心肌细胞。
背景:心肌递送不可兴奋细胞-即人间充质干细胞(hMSCs)和c-kit+心脏间质细胞(hcic)-仍然是治疗心力衰竭的一种有希望的方法。最近的实证研究试图通过基因工程细胞来表达特定的离子通道,或者通过创造混合通道表达的杂交细胞来改善这种疗法。本研究使用计算建模方法来验证一个假设,即当与人类心力衰竭(HF)心肌细胞结合时,可以合理地设计定制的假设细胞来恢复健康的表型。方法:用非兴奋性细胞和健康人心肌细胞(hCMs)的离子通道组合模拟候选定制细胞。使用基于遗传算法的优化方法,如果处理过的心衰心肌细胞的动作电位和钙瞬态波形相对于健康hCM的均方根误差(RMSE)小于50%,则接受候选细胞,并将其归一化为未处理的心衰心肌细胞。结果:当与纤维化或非纤维化HF心肌细胞偶联时,仅表达不可兴奋离子通道的定制细胞不足以恢复健康的心脏表型。相反,当与纤维化而非非纤维化HF心肌细胞偶联时,也表达心脏离子通道的定制细胞可导致健康心肌细胞表型的可接受恢复。合并心肌细胞内向整流K+通道对于完成这种表型拯救至关重要,同时也改善了与心律失常相关的单细胞动作电位指标,即静息膜电位和动作电位持续时间。计算方法还提供了对拯救机制的见解,即异细胞偶联增强心肌细胞l型钙电流并促进钙诱导的钙释放。最后,作为一种治疗上可翻译的策略,我们模拟了hMSCs和hCICs的传递,通过基因工程表达心肌细胞内向整流K+通道,相对于对照hMSCs和hCICs,其动作电位和钙瞬态rmse降低了至少24%,具有更有利的单细胞心律失常指标。结论:计算模型有助于探索可定制的工程细胞疗法。表达心脏离子通道的优化细胞恢复了纤维化HF心肌细胞的健康动作电位和钙处理表型,并改善了单细胞心律失常指标,需要对拟议的定制治疗细胞进行进一步的实验验证研究。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


