Obesity and hypovitaminosis D: causality or casualty?
引用次数: 101
Abstract
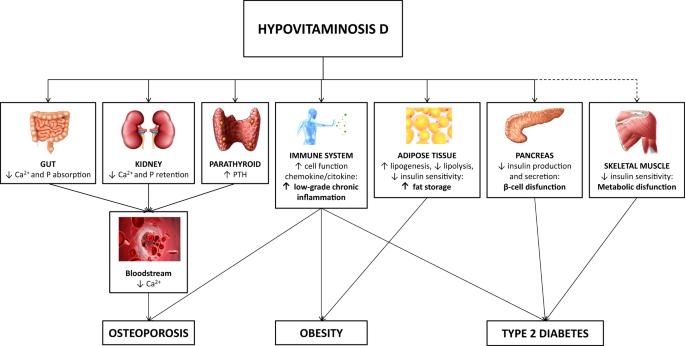
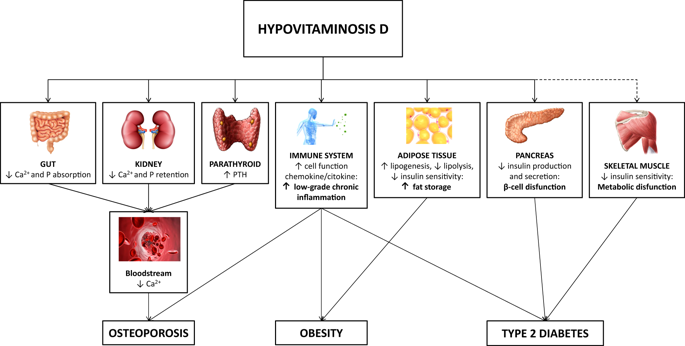
Epidemiological studies reported that vitamin D deficiency represents an increasingly widespread phenomenon in various populations. Vitamin D deficiency is considered a clinical syndrome determined by low circulating levels of 25-hydroxyvitamin D (25(OH)D), which is the biologically-inactive intermediate and represents the predominant circulating form. Different mechanisms have been hypothesized to explain the association between hypovitaminosis D and obesity, including lower dietary intake of vitamin D, lesser skin exposure to sunlight, due to less outdoor physical activity, decreased intestinal absorption, impaired hydroxylation in adipose tissue and 25(OH)D accumulation in fat. However, several studies speculated that vitamin D deficiency itself could cause obesity or prevent weight loss. The fat-solubility of vitamin D leads to the hypothesis that a sequestration process occurs in body fat depots, resulting in a lower bioavailability in the obese state. After investigating the clinical aspects of vitamin D deficiency and the proposed mechanisms for low 25(OH)D in obesity, in this manuscript we discuss the possible role of vitamin D replacement treatment, with different formulations, to restore normal levels in individuals affected by obesity, and evaluate potential positive effects on obesity itself and its metabolic consequences. Food-based prevention strategies for enhancement of vitamin D status and, therefore, lowering skeletal and extra-skeletal diseases risk have been widely proposed in the past decades; however pharmacological supplementation, namely cholecalciferol and calcifediol, is required in the treatment of vitamin D insufficiency and its comorbidities. In individuals affected by obesity, high doses of vitamin D are required to normalize serum vitamin D levels, but the different liposolubility of different supplements should be taken into account. Although the results are inconsistent, some studies reported that vitamin D supplementation may have some beneficial effects in people with obesity.
肥胖与维生素 D 不足:因果关系还是偶然因素?
流行病学研究报告显示,维生素 D 缺乏症在不同人群中日益普遍。维生素 D 缺乏症被认为是一种临床综合征,由循环中 25-羟基维生素 D(25(OH)D)水平低所决定,25-羟基维生素 D 是生物活性中间体,是循环中的主要形式。人们提出了不同的机制来解释维生素 D 过低与肥胖之间的关系,其中包括维生素 D 的膳食摄入量较低、户外运动较少导致皮肤接触阳光较少、肠道吸收减少、脂肪组织中的羟化作用受损以及 25(OH)D 在脂肪中的积累。不过,有几项研究推测,缺乏维生素 D 本身会导致肥胖或阻止体重减轻。由于维生素 D 具有脂溶性,因此有一种假设认为,体内脂肪库中会发生螯合过程,导致肥胖状态下的生物利用率降低。在研究了维生素 D 缺乏症的临床方面以及肥胖症中 25(OH)D 偏低的拟议机制后,我们在本手稿中讨论了不同配方的维生素 D 替代治疗在恢复肥胖症患者正常水平方面可能发挥的作用,并评估了对肥胖症本身及其代谢后果的潜在积极影响。过去几十年来,人们广泛提出了以食物为基础的预防策略,以改善维生素 D 状态,从而降低骨骼和骨骼外疾病的风险;然而,在治疗维生素 D 不足及其并发症时,需要补充药物,即胆钙化醇和降钙素。对于肥胖症患者,需要大剂量的维生素 D 才能使血清维生素 D 水平恢复正常,但应考虑到不同补充剂的脂溶性不同。尽管研究结果并不一致,但一些研究报告称,补充维生素 D 可能对肥胖症患者有益。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


