Understanding rural-urban differences in veterans’ internet access, use and patient preferences for telemedicine
Abstract
Background
The expansion of telemedicine (e.g., telephone or video) in the Veterans Health Administration (VA) raises concerns for health care disparities between rural and urban veterans. Factors impeding telemedicine use (e.g., broadband, digital literacy, age) disproportionally affect rural veterans.
Purpose
To examine veteran-reported broadband access, internet use, familiarity with, and preferences for telemedicine stratified by residential rurality.
Methods
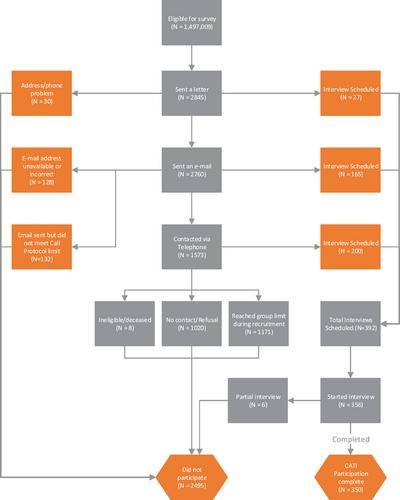
Three hundred fifty veterans with a VA primary care visit in March 2022 completed a 30-min computer-assisted telephone interview. The sampling design stratified veterans by residential rurality (i.e., rural or urban) and how primary care was delivered (i.e., in-person or by video). Counts and weighted percentages are reported.
Findings
After accounting for survey weights, 96.2% of respondents had in-home internet access and 89.5% reported functional connection speeds. However, rural- compared to urban-residing veterans were less likely to experience a telemedicine visit in the past year (74.1% vs. 85.2%; p = 0.02). When comparing telemedicine to in-person visits, rural versus urban-residing veterans rated them not as good (45.3% vs. 36.8%), just as good (51.1% vs. 53.1%), or better (3.5% vs. 10.0%) (p = 0.05). To make telemedicine visits easier, veterans, regardless of where they lived, recommended technology training (46.4%), help accessing the internet (26.1%), or provision of an internet-enabled device (25.9%).
Conclusions
Though rural-residing veterans were less likely to experience a telemedicine visit, the same actionable facilitators to improve telemedicine access were reported regardless of residential rurality. Importantly, technology training was most often recommended. Policy makers, patient advocates, and other stakeholders should consider novel initiatives to provide training resources.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


