下载PDF
{"title":"Buds, clusters, and transitions in 21st century colorectal carcinoma: revolution or reinvention?†","authors":"Roger M Feakins, Maurice B Loughrey, Andrew Silver","doi":"10.1002/path.6173","DOIUrl":null,"url":null,"abstract":"<p>Tumour budding (TB) describes single or small groups of neoplastic cells that lack continuity with an advancing tumour front. Poorly differentiated clusters (PDCs) are larger and qualitatively different. TB grade and PDCs may predict a worse outcome in colorectal carcinoma and other cancers and fall into the category of ‘invasive front prognostic markers’ that also includes intratumoural stroma type. Epithelial–mesenchymal transition (EMT) allows the adoption by epithelial cells of mesenchymal characteristics such as dyscohesion, migration, and stromal invasion. TB and PDCs harbor alterations in EMT-related proteins and RNAs and may be morphological manifestations of EMT. However, persistence of epithelioid features and absence of a full complement of typical alterations in TB and PDCs may indicate ‘partial EMT’, i.e. an intermediate/hybrid state. Recently, Pavlič <i>et al</i> asserted that TB and PDCs in colorectal cancer represent different manifestations of partial EMT and, perhaps controversially, that TB is closer than PDCs to complete transition. In clinical practice, low inter-observer agreement for invasive front prognostic markers is a potential problem. The UK colorectal cancer pathology dataset advises assessment of TB and recommends the use of an international consensus system, but time will tell if we are adopting reliable prognostic markers or reinventing the wheel. Additional studies of TB, PDCs, and EMT will presumably allow greater insight into their role in tumour development and progression. © 2023 The Authors. <i>The Journal of Pathology</i> published by John Wiley & Sons Ltd on behalf of The Pathological Society of Great Britain and Ireland.</p>","PeriodicalId":232,"journal":{"name":"The Journal of Pathology","volume":"261 2","pages":"121-124"},"PeriodicalIF":5.6000,"publicationDate":"2023-08-11","publicationTypes":"Journal Article","fieldsOfStudy":null,"isOpenAccess":false,"openAccessPdf":"https://onlinelibrary.wiley.com/doi/epdf/10.1002/path.6173","citationCount":"0","resultStr":null,"platform":"Semanticscholar","paperid":null,"PeriodicalName":"The Journal of Pathology","FirstCategoryId":"3","ListUrlMain":"https://onlinelibrary.wiley.com/doi/10.1002/path.6173","RegionNum":2,"RegionCategory":"医学","ArticlePicture":[],"TitleCN":null,"AbstractTextCN":null,"PMCID":null,"EPubDate":"","PubModel":"","JCR":"Q1","JCRName":"ONCOLOGY","Score":null,"Total":0}
引用次数: 0
引用
批量引用
Abstract
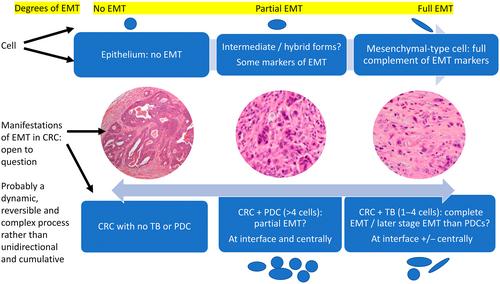
Tumour budding (TB) describes single or small groups of neoplastic cells that lack continuity with an advancing tumour front. Poorly differentiated clusters (PDCs) are larger and qualitatively different. TB grade and PDCs may predict a worse outcome in colorectal carcinoma and other cancers and fall into the category of ‘invasive front prognostic markers’ that also includes intratumoural stroma type. Epithelial–mesenchymal transition (EMT) allows the adoption by epithelial cells of mesenchymal characteristics such as dyscohesion, migration, and stromal invasion. TB and PDCs harbor alterations in EMT-related proteins and RNAs and may be morphological manifestations of EMT. However, persistence of epithelioid features and absence of a full complement of typical alterations in TB and PDCs may indicate ‘partial EMT’, i.e. an intermediate/hybrid state. Recently, Pavlič et al asserted that TB and PDCs in colorectal cancer represent different manifestations of partial EMT and, perhaps controversially, that TB is closer than PDCs to complete transition. In clinical practice, low inter-observer agreement for invasive front prognostic markers is a potential problem. The UK colorectal cancer pathology dataset advises assessment of TB and recommends the use of an international consensus system, but time will tell if we are adopting reliable prognostic markers or reinventing the wheel. Additional studies of TB, PDCs, and EMT will presumably allow greater insight into their role in tumour development and progression. © 2023 The Authors. The Journal of Pathology published by John Wiley & Sons Ltd on behalf of The Pathological Society of Great Britain and Ireland.
21世纪结直肠癌的萌芽、集群和转变:革命还是再造?†
肿瘤出芽(TB)描述了单个或小组肿瘤细胞,它们与前进的肿瘤前沿缺乏连续性。差分化集群(PDC)更大,质量也有所不同。TB分级和PDCs可能预测结直肠癌和其他癌症的预后更差,属于“侵袭性前沿预后标志物”类别,也包括肿瘤内基质类型。上皮-间充质转化(EMT)允许上皮细胞采用间充质特征,如内聚力失调、迁移和基质侵袭。TB和PDCs携带EMT相关蛋白和RNA的改变,可能是EMT的形态学表现。然而,上皮样特征的持续存在以及TB和PDCs典型改变的完整补充缺失可能表明“部分EMT”,即中间/混合状态。最近,Pavlič等人断言,结直肠癌癌症中的TB和PDC代表了部分EMT的不同表现,并且,也许有争议的是,TB比PDC更接近于完成转变。在临床实践中,侵入性前沿预后标志物的观察者间一致性低是一个潜在的问题。英国癌症结直肠病理数据集建议对结核病进行评估,并建议使用国际共识系统,但时间会告诉我们是采用可靠的预后标志物还是重新发明轮子。对结核病、PDCs和EMT的进一步研究可能会让人们更深入地了解它们在肿瘤发展和进展中的作用。©2023作者。病理学杂志由John Wiley&;代表大不列颠及爱尔兰病理学会的Sons有限公司。
本文章由计算机程序翻译,如有差异,请以英文原文为准。

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


