Intestinal overgrowth of Candida albicans exacerbates bleomycin-induced pulmonary fibrosis in mice with dysbiosis
IF 5.6
2区 医学
Q1 ONCOLOGY
引用次数: 0
Abstract
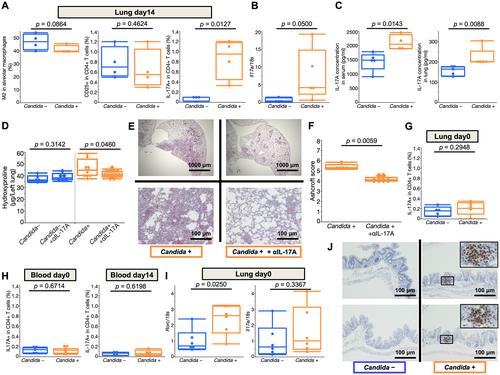
Increasing evidence indicates an interaction between the intestinal microbiota and diseases in distal organs. However, the relationship between pulmonary fibrosis and the intestinal microbiota, especially intestinal fungal microbiota, is poorly understood. Thus, this study aimed to determine the effects of changes in the intestinal fungal microbiota on the pathogenesis of pulmonary fibrosis. Mice with intestinal overgrowth of Candida albicans, which was established by oral administration of antibiotics plus C. albicans, showed accelerated bleomycin‐induced pulmonary fibrosis relative to the control mice (i.e. without C. albicans treatment). In addition, the mice with intestinal overgrowth of C. albicans showed enhanced Th17‐type immunity, and treatment with IL‐17A‐neutralizing antibody alleviated pulmonary fibrosis in these mice but not in the control mice. This result indicates that IL‐17A is involved in the pathogenesis of C. albicans‐exacerbated pulmonary fibrosis. Even before bleomycin treatment, the expression of Rorc, the master regulator of Th17, was already upregulated in the pulmonary lymphocytes of the mice with intestinal overgrowth of C. albicans. Subsequent administration of bleomycin triggered these Th17‐skewed lymphocytes to produce IL‐17A, which enhanced endothelial–mesenchymal transition. These results suggest that intestinal overgrowth of C. albicans exacerbates pulmonary fibrosis via IL‐17A‐mediated endothelial–mesenchymal transition. Thus, it might be a potential therapeutic target in pulmonary fibrosis. This study may serve as a basis for using intestinal fungal microbiota as novel therapeutic targets in pulmonary fibrosis. © 2023 The Authors. The Journal of Pathology published by John Wiley & Sons Ltd on behalf of The Pathological Society of Great Britain and Ireland.
肠道白色念珠菌过度生长加剧博莱霉素诱导的肺纤维化失调小鼠
越来越多的证据表明,肠道微生物群与远端器官疾病之间存在相互作用。然而,肺纤维化与肠道菌群,特别是肠道真菌菌群之间的关系尚不清楚。因此,本研究旨在确定肠道真菌菌群的变化对肺纤维化发病机制的影响。通过口服抗生素和白色念珠菌建立了肠道白色念珠菌过度生长的小鼠,与对照小鼠(即没有白色念珠菌治疗)相比,博莱霉素诱导的肺纤维化加速。此外,肠道白色念珠菌过度生长的小鼠表现出增强的th17型免疫,il - 17a中和抗体治疗减轻了这些小鼠的肺纤维化,而对照组小鼠则没有。提示IL-17A参与了白念珠菌加重肺纤维化的发病机制。即使在博来霉素治疗之前,Th17的主要调控因子Rorc在肠道白色念珠菌过度生长小鼠的肺淋巴细胞中的表达就已经上调。随后给予博来霉素触发这些th17倾斜的淋巴细胞产生IL-17A,从而增强内皮-间质转化。这些结果表明,肠道白色念珠菌的过度生长通过il - 17a介导的内皮-间质转化加剧了肺纤维化。因此,它可能是肺纤维化的潜在治疗靶点。本研究可为利用肠道真菌菌群作为肺纤维化治疗的新靶点提供基础。©2023作者。《病理学杂志》由约翰·威利出版;儿子有限公司代表大不列颠及爱尔兰病理学会。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

The Journal of Pathology
医学-病理学
CiteScore
14.10
自引率
1.40%
发文量
144
审稿时长
3-8 weeks
期刊介绍:
The Journal of Pathology aims to serve as a translational bridge between basic biomedical science and clinical medicine with particular emphasis on, but not restricted to, tissue based studies. The main interests of the Journal lie in publishing studies that further our understanding the pathophysiological and pathogenetic mechanisms of human disease.
The Journal of Pathology welcomes investigative studies on human tissues, in vitro and in vivo experimental studies, and investigations based on animal models with a clear relevance to human disease, including transgenic systems.
As well as original research papers, the Journal seeks to provide rapid publication in a variety of other formats, including editorials, review articles, commentaries and perspectives and other features, both contributed and solicited.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


