In-hospital deprescribing in the real world – a clinician-led approach to hyperpolypharmacy
Abstract
Background
A lack of clear guidelines for medication cessation has contributed to the proliferation of polypharmacy. Hospitalisation provides a unique opportunity for initiating deprescribing. Deprescribing interventions are usually pharmacist- or multidisciplinary team-led and are typically safe and beneficial for patients. However, few studies have explored interventions that are implementable by clinicians at the bedside.
Aim
To explore the efficacy and feasibility of a clinician-led deprescribing intervention on an acute general medicine ward.
Method
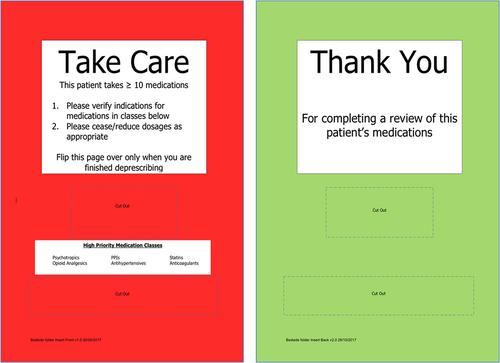
A multifaceted intervention was implemented comprising (a) education sessions on deprescribing and (b) a deprescribing alert in the bedside folders of patients with hyperpolypharmacy (>10 medications). Using a historical cohort study design, data from the intervention cohort were compared to a historical control group. A subset of the intervention cohort was surveyed after discharge regarding attitudes toward deprescribing.
Results
We recruited 1333 patients and had complete data for 1169 (nintervention = 888, ncontrol = 281). The prevalence of hyperpolypharmacy decreased from 28% to 26% in the intervention cohort, but this reduction was not statistically significant (net change = −1, interquartile range [IQR] = −2–0; p = 0.26). There was similarly no statistically significant change in medication numbers due to the intervention across other subgroups. Most patients agreed they were taking too many medications and supported deprescribing.
Conclusions
Despite observing no statistically significant effect of the intervention, we demonstrated the feasibility of introducing clinician-led deprescribing interventions in resource-poor, busy inpatient units. Simple, innovative deprescribing interventions in hospital settings, along with the measurement of long-term patient outcomes and medication adverse effects, should be investigated further in large inpatient cohorts.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


