Evaluation of sweating responses in patients with systemic connective tissue disorders using the quantitative sudomotor axon reflex test
Abstract
Background
In systemic connective tissue disorders, eccrine sweat glands are frequently attacked by immune cells, as evidenced by pathological observations.
Aims
Sweating affects vascular activity through the autonomic nervous system, while few studies have reported sweating ability in systemic connective tissue disorders or the relationship between sweating ability and Raynaud's phenomenon caused by sympathetic hyperreactivity.
Materials & methods
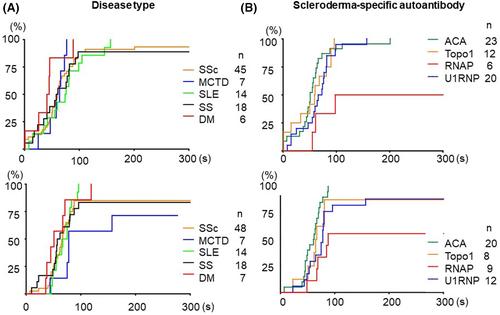
We performed the quantitative sudomotor axon reflex test on 85 patients diagnosed with systemic sclerosis, mixed connective tissue disease, systemic lupus erythematosus, Sjogren's syndrome, and dermatomyositis. Evaluations were performed once in summer and once in winter. We investigated the relationship between the axon reflex sweat volume or the reaction time and Raynaud's phenomenon assessed by a Raynaud's condition score, skin symptoms such as nailfold capillary changes, skin sclerosis severity, digital ulcers, chilblains, subcutaneous calcifications, and telangiectasia, and patient background.
Results
Most patients did not show a decrease in sweating compared to healthy participants, but patients with systemic sclerosis who were positive for anti-RNA polymerase III antibodies showed little or no sweating. One in three patients showed less sweating in summer than in winter, which is the opposite of the normal seasonal variation. Although no relationship was observed between the sweat volume and the total Raynaud's condition scores, patients with pain had more sweating than those without pain.
Conclusion
This is the first exploratory observational study of sweating ability in patients with systemic connective tissue disorders, revealing several clinical factors associated with acetylcholine-induced sweating.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


