Combining familial hypercholesterolemia and statin genetic studies as a strategy for the implementation of pharmacogenomics. A multidisciplinary approach
IF 2.9
3区 医学
Q2 GENETICS & HEREDITY
引用次数: 0
Abstract
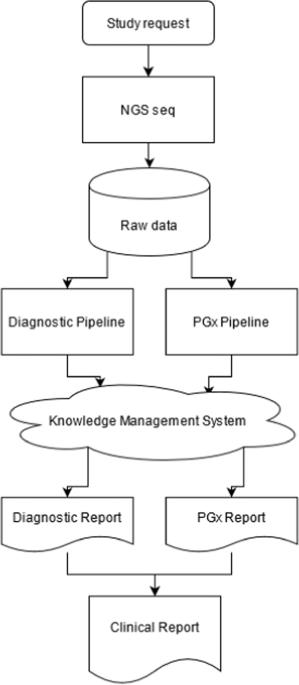
The diagnostic process of familial hypercholesterolemia frequently involves the use of genetic studies. Patients are treated with lipid-lowering drugs, frequently statins. Although pharmacogenomic clinical practice guidelines focusing on genotype-based statin prescription have been published, their use in routine clinical practice remains very modest. We have implemented a new NGS strategy that combines a panel of genes related to familial hypercholesterolemia with genomic regions related to the pharmacogenomics of lipid-lowering drugs described in clinical practice guidelines and in EMA and FDA drug labels. A multidisciplinary team of doctors, biologists, and pharmacists creates a clinical report that provides diagnostic and therapeutic findings using a knowledge management and clinical decision support system, as well as an algorithm for treatment selection. For 12 months, a total of 483 genetic diagnostic studies for familial hypercholesterolemia were carried out, of which 221 (45.8%) requested a complementary pharmacogenomic test. Of these 221 patients, 66.5% were carriers of actionable variants in any of the studied pharmacogenomic pathways: 46.6% of patients in one pathway, 19.0% in two pathways, and 0.9% in three pathways. 45.7% of patients could have a response to atorvastatin different from that of the reference population, 45.7% for simvastatin and lovastatin, 29.0% for fluvastatin, and 6.7% patients for pitavastatin. This implementation approach facilitates the incorporation of pharmacogenomic studies in clinical care practice, it does not add complexity nor additional steps to laboratory processes, and improves the pharmacotherapeutic process of patients.
结合家族性高胆固醇血症和他汀类药物基因研究作为药物基因组学实施策略。多学科方法
家族性高胆固醇血症的诊断过程经常涉及基因研究。患者接受降脂药物治疗,通常是他汀类药物。虽然已经发布了以基因型为基础的他汀类药物处方为重点的药物基因组学临床实践指南,但其在常规临床实践中的应用仍然非常有限。我们采用了一种新的 NGS 策略,将家族性高胆固醇血症相关基因与临床实践指南以及 EMA 和 FDA 药物标签中描述的降脂药物药物基因组学相关基因组区域相结合。由医生、生物学家和药剂师组成的多学科团队利用知识管理和临床决策支持系统以及治疗选择算法创建临床报告,提供诊断和治疗结果。在 12 个月中,共进行了 483 次家族性高胆固醇血症基因诊断研究,其中 221 人(45.8%)要求进行补充药物基因组学检测。在这 221 名患者中,66.5% 是所研究的药物基因组学途径中可操作变异的携带者:46.6%的患者为一种途径变异携带者,19.0%为两种途径变异携带者,0.9%为三种途径变异携带者。45.7%的患者对阿托伐他汀的反应可能不同于参照人群,45.7%的患者对辛伐他汀和洛伐他汀的反应不同于参照人群,29.0%的患者对氟伐他汀的反应不同于参照人群,6.7%的患者对匹伐他汀的反应不同于参照人群。这种实施方法有助于将药物基因组学研究纳入临床护理实践,既不会增加实验室流程的复杂性,也不会增加额外的步骤,还能改善患者的药物治疗过程。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Pharmacogenomics Journal
医学-药学
CiteScore
7.20
自引率
0.00%
发文量
35
审稿时长
6-12 weeks
期刊介绍:
The Pharmacogenomics Journal is a print and electronic journal, which is dedicated to the rapid publication of original research on pharmacogenomics and its clinical applications.
Key areas of coverage include:
Personalized medicine
Effects of genetic variability on drug toxicity and efficacy
Identification and functional characterization of polymorphisms relevant to drug action
Pharmacodynamic and pharmacokinetic variations and drug efficacy
Integration of new developments in the genome project and proteomics into clinical medicine, pharmacology, and therapeutics
Clinical applications of genomic science
Identification of novel genomic targets for drug development
Potential benefits of pharmacogenomics.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


