Severe efavirenz associated neurotoxicity: A retrospective cohort study.
IF 1.3
Q4 INFECTIOUS DISEASES
Southern African Journal of Infectious Diseases
Pub Date : 2023-07-24
eCollection Date: 2023-01-01
DOI:10.4102/sajid.v38i1.522
引用次数: 0
Abstract
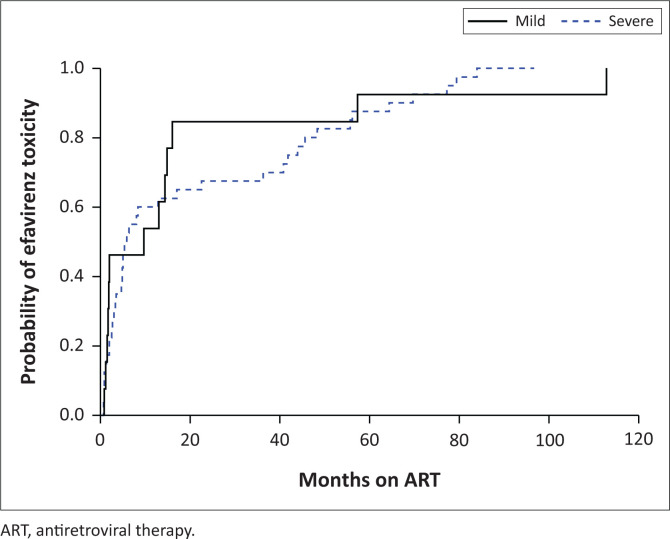
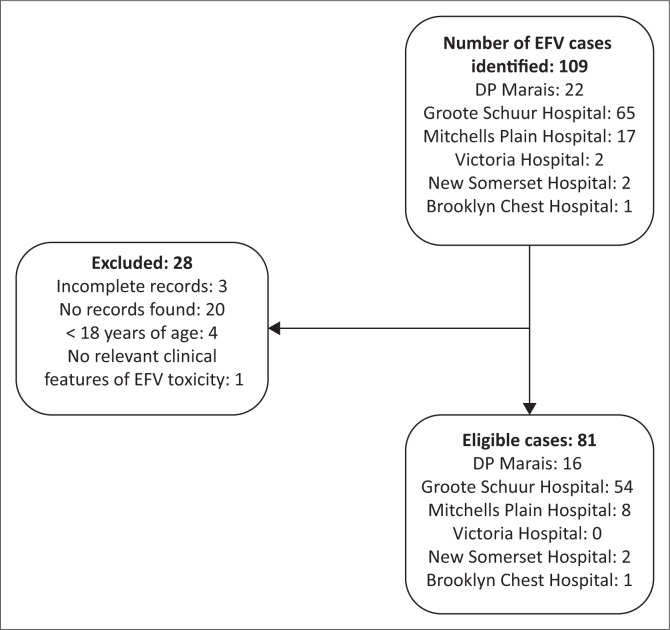
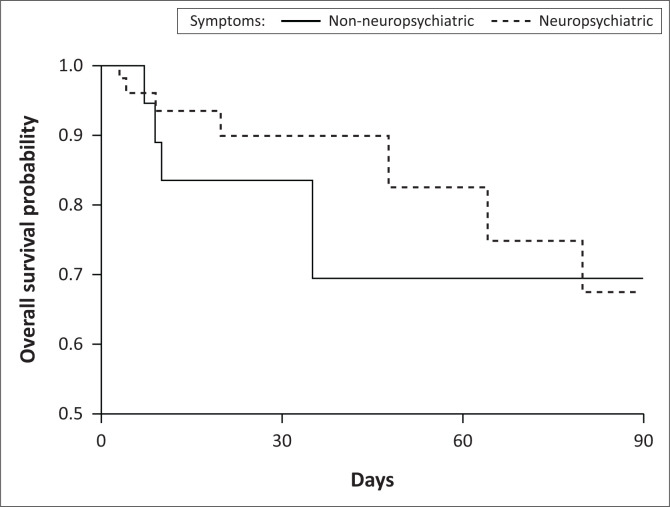
Background Efavirenz (EFV) is associated with neuropsychiatric symptoms. Severe neurotoxicity has been reported but the clinical phenotype and risk factors are poorly defined. Objectives To characterise clinical presentations, risk factors and outcomes to help clinicians recognise severe neurotoxicity earlier. Method The authors retrospectively identified adults with supratherapeutic EFV concentrations (> 4 mg/L) obtained during routine clinical care in Cape Town, South Africa. Clinical and laboratory data at the time of EFV quantification were extracted from medical records. Logistic regression was performed to identify associations with neuropsychiatric symptoms, and with severe neurotoxicity. Results Eighty one patients were included; 62 with neuropsychiatric manifestations (most frequently ataxia [n = 20] and psychomotor slowing [n = 24]); and 19 with hepatotoxicity. Overall, 28 (34.6%) were male, 49 (60.5%) had concomitant isoniazid exposure, and median EFV concentration was 12.1 mg/L (interquartile range [IQR]: 6.6–20.0). Neuropsychiatric symptoms were associated with longer duration of EFV therapy, adjusted odds ratio (aOR) 1.3/180-day increment (95% confidence interval [CI]: 1.0–1.7); higher EFV concentrations, aOR 1.2/1 mg/L increase (95% CI: 1.0–1.4) and isoniazid exposure, aOR 8.2 (95% CI: 2.5–26.7). Severe neuropsychiatric symptoms occurred in 47 (75%) patients at a median of 5.9 months (IQR: 2.1–40.8) after EFV initiation. Severe symptoms odds were 1.2-fold higher (95% CI: 1.1–1.4) per 1 mg/L increase in EFV concentration. Symptoms resolved completely within 1 month in 25 (76%) patients with severe neurotoxicity who discontinued EFV. Conclusion A concentration–effect relationship for severe neurotoxicity exists, which occurred late and resolved in most patients after EFV discontinuation. Contribution The authors highlighted clinical heterogeneity and morbidity of EFV-associated neurotoxicity.
严重依非韦伦相关神经毒性:一项回顾性队列研究。
背景:依非韦仑(EFV)与神经精神症状有关。严重的神经毒性已有报道,但临床表型和危险因素尚不明确。目的:描述临床表现、危险因素和结果,以帮助临床医生更早地识别严重的神经毒性。方法:作者回顾性地确定了在南非开普敦的常规临床护理中获得的超治疗性EFV浓度(>4 mg/L)的成年人。从医疗记录中提取EFV定量时的临床和实验室数据。进行Logistic回归以确定与神经精神症状和严重神经毒性的相关性。结果:纳入81例患者;62例有神经精神表现(最常见的是共济失调[n=20]和精神运动迟缓[n=24]);肝毒性19例。总体而言,28例(34.6%)为男性,49例(60.5%)同时接触异烟肼,EFV的中位浓度为12.1 mg/L(四分位间距[IQR]:6.6-20.0)。神经精神症状与EFV治疗持续时间更长、调整比值比(aOR)1.3/180天增加(95%置信区间[CI]:1.0-1.7)有关;EFV浓度越高,aOR增加1.2/1 mg/L(95%CI:1.0-1.4),异烟肼暴露,aOR 8.2(95%CI:2.5-26.7)。47名(75%)患者在EFV开始后的中位5.9个月(IQR:2.1-40.8)出现严重的神经精神症状。EFV浓度每增加1 mg/L,出现严重症状的几率就高出1.2倍(95%可信区间:1.1-1.4)。25例(76%)严重神经毒性患者停用EFV后,症状在1个月内完全缓解。结论:严重神经毒性存在浓度-效应关系,这种关系发生得较晚,大多数患者在EFV停用后症状缓解。贡献:作者强调了EFV相关神经毒性的临床异质性和发病率。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Southern African Journal of Infectious Diseases
INFECTIOUS DISEASES-
自引率
11.10%
发文量
50
审稿时长
52 weeks
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


