Development of normalized quantitative measures of lumbar disc degeneration
Abstract
Background
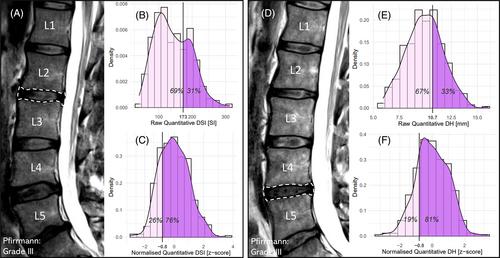
Lumbar disc degeneration (DD) is widely regarded as a likely contributor to low back pain (LBP), but the association between DD and LBP is relatively weak. No known studies have normalized quantitative measures of DD severity relative to multiple variables such as age, height, and disc level. This study developed normalized quantitative measures (z-scores) of disc signal intensity (DSI) and disc height (DH) to rate relative severity of DD.
Methods
Raw (unnormalized) quantitative measures of DSI and DH alongside potential normalization variables were acquired from MRI scans and clinical data of 76 patients. The associations between the raw quantitative measures and potential normalization variables were investigated to develop the normalized quantitative measures (z-scores) of DSI and DH. Construct validity was assessed by comparing the normalized measures to an experienced radiologist's subjective measures of relative severity of DSI and DH loss.
Results
CSF signal intensity, age, and disc level were significantly associated with raw DSI (R2 = 0.06, 0.25, and 0.09, respectively). Lumbar height and disc level were significantly associated with raw DH (R2 = 0.13 and 0.31). Normalizing DSI and DH by these variables resulted in stronger relationships (R2 = 0.39 and 0.37) than raw DSI and DH (R2 = 0.24 and 0.31) with the radiologist's subjective measures. Normalized DSI and DH were both normally distributed (p = 0.32 and 0.12).
Conclusions
Construct validity and the distributions suggested that normalized quantitative measures of DSI and DH are better than existing measures of DSI and DH at rating relative DD severity. Determining whether normalized quantitative measures are more predictive of clinical outcomes is important future research.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


