Preconditions that facilitate cannulation in arteriovenous fistula: A mixed-methods study
Abstract
Background
Nurses have a great responsibility in the daily care of arteriovenous fistulae, which entails the potential to affect patency. However, good cannulation technique involves more than placing a needle in the vessel and relies on different skills to facilitate needling.
Objectives
To describe the preconditions for cannulation in arteriovenous fistulas.
Design
Descriptive statistics and qualitative content analysis were used in a mixed-methods design.
Participants
Haemodialysis units in Sweden.
Measurements
Local guidelines regarding arteriovenous fistula cannulation were analysed in parallel with responses to a questionnaire that contained open-ended and closed-ended questions on cannulation technique.
Results
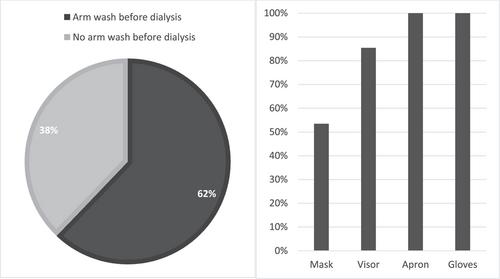
Preconditions that facilitate cannulation fall into five stages, each with relevant factors in relation to the cannulation, as follows: planning cannulation—maturation and planning the cannulation, patient record, education and experience, and patient information; precannulation—physical examination, hygiene routines, arm position, tourniquet, choosing the cannulation site, and preventing pain; during cannulation—how to needle, type of needle, angle during cannulation, fixation, and adjusting; evaluating cannulation—blood flow rate and arterial and venous pressure; and postcannulation—needle withdrawal and haemostasis. The majority of dialysis units identified implementation of most of these preconditions, but the units handle several practical aspects differently.
Conclusions
Tracing the chain of cannulation led to identification of necessary preconditions for facilitating good cannulation technique. The findings also show the need for a better understanding of how different preconditions affect arteriovenous fistula and patency.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


