Successful Treatment of Post-Myocardial Infarction Ventricular Septal Rupture.
International Journal of Heart Failure
Pub Date : 2021-05-18
eCollection Date: 2021-07-01
DOI:10.36628/ijhf.2021.0004
引用次数: 1
Abstract
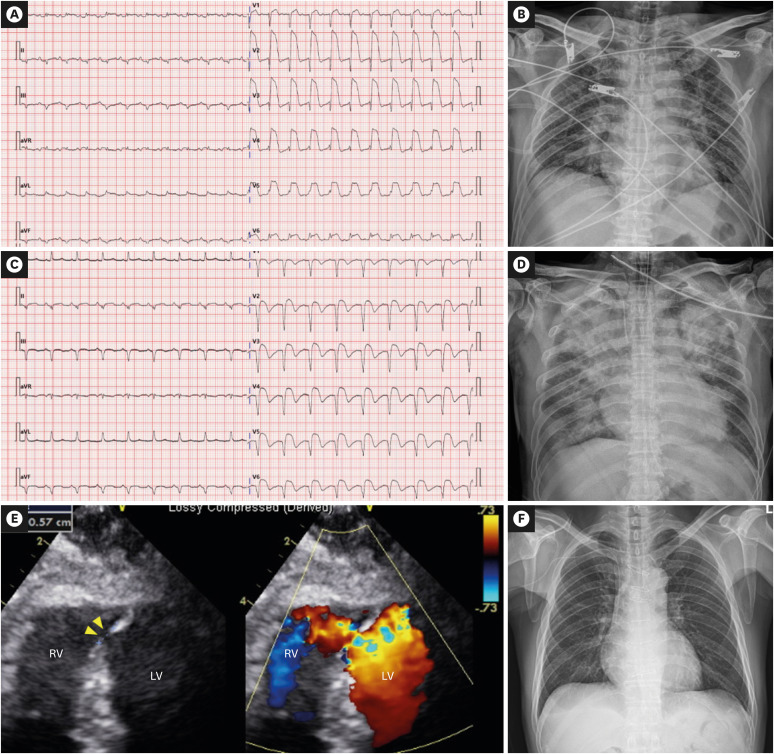
https://e-heartfailure.org A 61-year-old man with no previous history visited the emergency room due to a sudden onset of chest pains since 2 days. Initial electrocardiography (ECG) showed a 15 mm ST segment elevation in precordial leads with pathologic Q waves (Figure 1A). Initial supine anteroposterior chest radiography showed cardiomegaly (cardiothoracic ratio 0.56) with pulmonary congestion (Figure 1B). Since the patient presented with hypotension (blood pressure: 78/62 mmHg) and persistent chest pain, emergency percutaneous coronary intervention was planned under the support of norepinephrine (0.1 μg/kg/min). The initial coronary angiography revealed total occlusion of the middle left anterior descending (LAD) artery (Supplementary Video 1). After successful implantation of a sirolimus-eluting stent (3×24 mm), angiography showed no-reflow phenomenon (Supplementary Video 2). Intracoronary nicorandil infusion and intravascular abciximab were administered, and TIMI flow of grade 1 was confirmed by follow-up angiography (Supplementary Video 3). Postprocedural ECG showed partially resolved ST segments, but abnormal Q waves persisted (Figure 1C). Laboratory findings revealed the following: creatine kinase-myocardial band, 110 ng/mL; Troponin I 59.4 ng/mL; lactic acid, 4.4 mmol/L; and total bilirubin, 1.63 mg/ dL. Transthoracic echocardiography (TTE) showed severely decreased left ventricular (LV) ejection fraction with akinesia of the anterior and septal walls and aneurysm formation of the apical wall. Color Doppler imaging revealed shunt flow at the apical portion of the interventricular septum due to ventricular septal rupture (VSR) (1.6 cm) (Figure 1E). Since the patient's pain was tolerable, and his vital signs and laboratory findings were stabilized without increment of positive inotropes (norepinephrine 0.1 μg/kg/min), our multidisciplinary cardiac team including a cardiac intensivist, cardiac surgeon, and cardiac imaging specialist, decided to delay surgery and closely monitor the patient at the cardiac intensive care unit. On the ninth day following admission, the patient reported worsening dyspnea. Chest radiography showed abrupt exacerbation of bilateral pulmonary edema and systolic blood pressure dropped under 90 mmHg, requiring additional norepinephrine infusion to 0.15 μg/kg/min (Figure 1D). Immediate extracorporeal membrane oxygenation (ECMO) was performed with mechanical ventilator support (Flow rate 3.8 liter per minute [LPM], 3565 revolution per minute [RPM], FiO2 0.65). Chest radiography confirmed the resolution of pulmonary edema. The patient's vital signs and laboratory findings were stabilized. However, on the sixth day of ECMO, lactic acid and bilirubin level increased to 6.5 mmol/L and 5.63 mg/dL, respectively, indicating progression of inadequate tissue perfusion and venous congestion despite the ECMO support. Conservative management such as diuretics and ursodeoxycholic acid use was not effective. Therefore, the heart team Int J Heart Fail. 2021 Jul;3(3):200-204 https://doi.org/10.36628/ijhf.2021.0004 pISSN 2636-154X·eISSN 2636-1558
心肌梗死后室间隔破裂的成功治疗。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


