A Case Report about Glycogenic Hepatopathy.
IF 0.9
Q4 ENDOCRINOLOGY & METABOLISM
Case Reports in Endocrinology
Pub Date : 2022-10-18
eCollection Date: 2022-01-01
DOI:10.1155/2022/5134049
引用次数: 0
Abstract
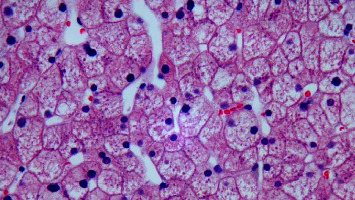
Introduction Glycogenic hepatopathy is a rare complication of uncontrolled diabetes mellitus that presents with hepatomegaly and transient elevation in serum aminotransferase enzymes. The underlying pathophysiology involves excessive accumulation of intrahepatic glycogen. Glycogenic hepatopathy is usually underdiagnosed because it is difficult to differentiate from other entities, such as the nonalcoholic fatty liver. The gold standard for diagnosis is liver biopsy. Glycogenic hepatopathy can be reversed by the achievement of adequate glycemic control. Case description. A 19-year-old female patient with a history of poorly controlled type 1 diabetes mellitus that resulted in several episodes of diabetes ketoacidosis requiring hospital admissions. The patient presented to the emergency room with generalized weakness and fatigue found to have diabetic ketoacidosis. Blood tests revealed abnormal liver function with aspartate aminotransferase 1129 U/L (13–37 U/L), alanine aminotransferase 766 U/L (13–56 U/L), alkaline phosphatase 216 U/L (45–117 U/L), total bilirubin 1.0 mg/dL (0.2–1.3 mg/dL), albumin 3.8 g/dL (3.4–5.0 g/dL), partial thromboplastin time < 20 s (23–31 s), prothrombin time 11.8 s (9.5–11.5 s), and international normalized ratio 1.1. Acute hepatitis serologies were negative. Epstein–Barr virus and cytomegalovirus were ruled out. Extensive autoimmune hepatitis tests were negative. Primary biliary cirrhosis was also ruled out. A liver biopsy was obtained, which was diagnostic of glycogenic hepatopathy. Conclusion Glycogenic hepatopathy must be suspected in patients with uncontrolled type 1 diabetes mellitus who present with elevated liver enzymes and hepatomegaly. Treating this rare condition requires a timely diagnosis with liver biopsy and strict glycemic control.
糖原性肝病1例报告。
糖原性肝病是糖尿病的一种罕见的并发症,表现为肝肿大和血清转氨酶的短暂升高。潜在的病理生理机制包括肝内糖原的过度积累。糖原性肝病通常诊断不足,因为很难与其他疾病(如非酒精性脂肪肝)区分。诊断的金标准是肝活检。糖原性肝病可以通过适当的血糖控制而逆转。案例描述。19岁女性患者,既往1型糖尿病控制不良,多次发生糖尿病酮症酸中毒,需住院治疗。患者以全身无力和疲劳就诊于急诊室,发现为糖尿病酮症酸中毒。血液检查显示肝功能异常,天冬氨酸转氨酶1129 U/L (13 ~ 37 U/L),丙氨酸转氨酶766 U/L (13 ~ 56 U/L),碱性磷酸酶216 U/L (45 ~ 117 U/L),总胆红素1.0 mg/dL (0.2 ~ 1.3 mg/dL),白蛋白3.8 g/dL (3.4 ~ 5.0 g/dL),部分凝血活素时间< 20 s (23 ~ 31 s),凝血酶原时间11.8 s (9.5 ~ 11.5 s),国际标准化比值1.1。急性肝炎血清学阴性。排除eb病毒和巨细胞病毒。广泛的自身免疫性肝炎试验呈阴性。原发性胆汁性肝硬化也被排除。行肝活检,诊断为糖原性肝病。结论:1型糖尿病未控制时出现肝酶升高和肝肿大的患者必须怀疑糖原性肝病。治疗这种罕见的疾病需要及时诊断,肝活检和严格的血糖控制。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Case Reports in Endocrinology
ENDOCRINOLOGY & METABOLISM-
CiteScore
2.10
自引率
0.00%
发文量
45
审稿时长
13 weeks
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


