A Case of Paediatric Anti-Glomerular Basement Membrane Disease Associated with Thrombotic Thrombocytopenic Purpura.
Case Reports in Nephrology
Pub Date : 2022-08-27
eCollection Date: 2022-01-01
DOI:10.1155/2022/2676696
引用次数: 2
Abstract
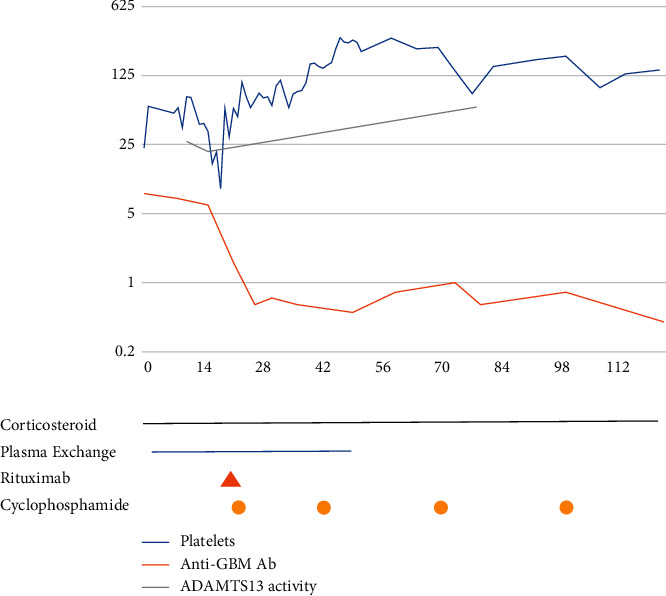
Anti-GBM disease is a rare vasculitis that causes rapid progressive glomerulonephritis and pulmonary haemorrhage. It is usually an adult diagnosis with isolated paediatric cases reported. Thrombotic thrombocytopenic purpura (TTP) is a rare thrombotic microangiopathy mainly affecting adults that causes multiorgan ischaemia, microangiopathic haemolytic anaemia, and thrombocytopenia. We present the first paediatric case of concurrent anti-GBM disease and TTP. A 14-year-old boy presented with acute kidney failure and severe pulmonary haemorrhage due to anti-GBM disease, confirmed on auto-antibody testing. There was thrombocytopenia and moderately low ADAMTS13 activity suggestive of TTP. The renal prognosis was poor with a need for dialysis. He was severely unwell with pulmonary haemorrhages requiring the use of extracorporeal membrane oxygenation (ECMO). His disease was treated with corticosteroids, plasma exchange (PEX), rituximab, and cyclophosphamide, resulting in remission. Anti-GBM disease is rare in children but should be considered in those presenting with acute kidney injury, particularly where there has been exposure to pulmonary irritants. An aggressive presentation warrants aggressive treatment with methylprednisolone, PEX, and cyclophosphamide. Rituximab may benefit patients that have concurrent TTP. TTP may exacerbate pulmonary disease, but complete respiratory recovery is possible. Disease relapse is rare in the paediatric age group, and these patients are candidates for kidney transplantation.

儿童抗肾小球基底膜病合并血栓性血小板减少性紫癜1例。
抗gbm疾病是一种罕见的血管炎,可引起快速进行性肾小球肾炎和肺出血。它通常是成人诊断,有孤立的儿科病例报告。血栓性血小板减少性紫癜(TTP)是一种罕见的血栓性微血管疾病,主要影响成人,可导致多器官缺血、微血管性溶血性贫血和血小板减少。我们提出的第一个儿科病例并发抗gbm疾病和TTP。一名14岁男孩因抗gbm疾病出现急性肾衰竭和严重肺出血,经自身抗体检测证实。有血小板减少和中等低的ADAMTS13活性提示TTP。肾脏预后差,需要透析。他严重不适,肺出血,需要体外膜氧合(ECMO)。他的疾病经皮质类固醇、血浆置换(PEX)、利妥昔单抗和环磷酰胺治疗后得到缓解。抗gbm疾病在儿童中很少见,但应考虑急性肾损伤患者,特别是暴露于肺部刺激物的患者。侵袭性表现需要甲泼尼龙、PEX和环磷酰胺的积极治疗。利妥昔单抗可能对并发TTP的患者有益。TTP可能加重肺部疾病,但完全恢复呼吸系统是可能的。疾病复发在儿科年龄组是罕见的,这些患者是肾移植的候选者。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


