The Association of Alcohol Use Disorder with Perioperative Complications following Primary Total Hip Arthroplasty.
引用次数: 4
Abstract
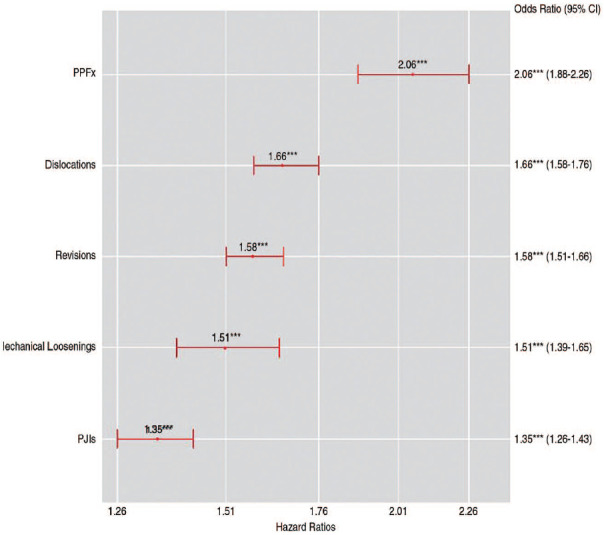
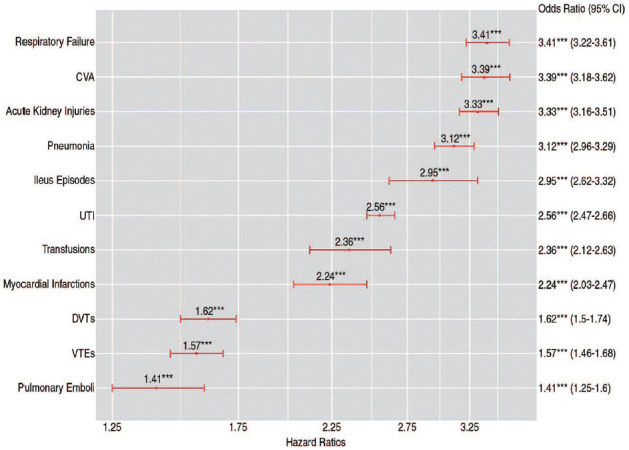
Purpose Alcohol use disorder is a leading mental health disorder in the United States. Few studies evaluating the association of alcohol use disorder following primary total hip arthroplasty (THA) have been reported. Therefore, the purpose of this study was to determine whether patients with alcohol use disorder undergoing primary THA have higher rates of: 1) in-hospital lengths of stay (LOS); 2) complications (medical/implant-related); and 3) costs. Materials and Methods Using a nationwide claims database from January 1st, 2005 to March 31st, 2014, patients with alcohol use disorder undergoing primary THA were identified and matched to a comparison group according to age, sex, and various comorbidities, resulting in 230,467 patients who were included in the study (n=38,416) and a matched-cohort (n=192,051). Outcomes of interest included comparison of LOS, 90-day medical and 2-year implant-related complications, and costs. A P-value less than 0.002 was considered statistically significant. Results Patients with alcohol use disorder had longer in-hospital LOS (4 days vs 3 days; P<0.0001) as well as higher frequency and odds ratio (OR) of 90-day medical (45.94% vs 12.25%; OR, 2.89; P<0.0001) and 2-year implant-related complications (17.71% vs 8.46%; OR, 1.97; P<0.0001). Patients in the study group incurred higher 90-day costs of care ($17,492.63 vs $14,921.88; P<0.0001). Conclusion With the growing prevalence of alcohol use disorder in the United States, the current investigation can be utilized to evaluate the need for interventions prior to THA which can potentially minimize the rates of morbidity and mortality within this population.

初次全髋关节置换术后酒精使用障碍与围手术期并发症的关系
目的:酒精使用障碍是美国主要的精神健康障碍。很少有研究评估原发性全髋关节置换术后酒精使用障碍的相关性。因此,本研究的目的是确定酒精使用障碍患者接受原发性THA是否有更高的发生率:1)住院时间(LOS);2)并发症(医疗/植入物相关);3)成本。材料和方法:使用2005年1月1日至2014年3月31日的全国索赔数据库,对接受原发性THA治疗的酒精使用障碍患者进行识别,并根据年龄、性别和各种合并症与对照组进行匹配,共纳入230,467例患者(n=38,416)和匹配队列(n=192,051)。结果包括LOS、90天医疗和2年种植体相关并发症和费用的比较。p值小于0.002被认为具有统计学意义。结果:酒精使用障碍患者的住院LOS较长(4天vs 3天;结论:随着美国酒精使用障碍的日益流行,目前的调查可以用来评估在全髋关节置换术之前进行干预的必要性,这可能会使这一人群的发病率和死亡率降到最低。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


