Through-and-Through Dissection of the Soft Palate for Pharyngeal Flap Inset: A "Good-Fast-Cheap" Technique for Any Etiology of Velopharyngeal Incompetence.
The Cleft palate-craniofacial journal : official publication of the American Cleft Palate-Craniofacial Association
Pub Date : 2022-06-01
Epub Date: 2021-06-17
DOI:10.1177/10556656211021738
引用次数: 3
Abstract
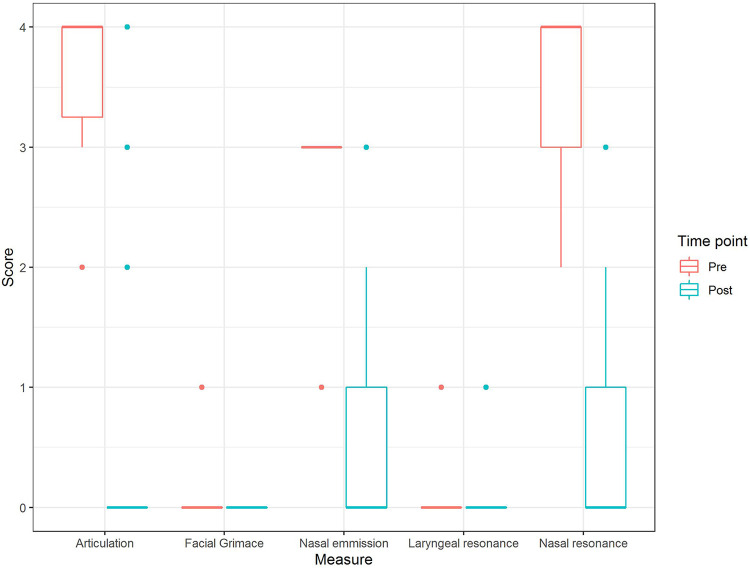
Objective: To determine the efficacy and resource utilization of through-and-through dissection of the soft palate for pharyngeal flap inset for velopharyngeal incompetence (VPI) of any indication. Design: Retrospective review. Setting: Tertiary care center. Patients: Thirty patients were included. Inclusion criteria were diagnosis of severe VPI based on perceptual speech assessment, confirmed by nasoendoscopy or videofluoroscopy; VPI managed surgically with modified pharyngeal flap with through-and-through dissection of the soft palate; and minimum 6 months follow-up. Patients with 22q11.2 deletion syndrome were excluded. Intervention: Modified pharyngeal flap with through-and-through dissection of the soft palate. Main Outcome Measure(s): Velopharyngeal competence and speech assessed using the Speech-Language Pathologist 3 scale. Results: The median preoperative speech score was 11 of 13 (range, 7 to 13), which improved significantly to a median postoperative score of 1 of 13 (range 0-7; P < .001). Velopharyngeal competence was restored in 25 (83%) patients, borderline competence in 3 (10%), and VPI persisted in 2 (7%) patients. Complications included 1 palatal fistula that required elective revision and 1 mild obstructive sleep apnea that did not require flap takedown. Median skin-to-skin operative time was 73.5 minutes, and median length of stay (LOS) was 50.3 hours. Conclusions: This technique allows direct visualization of flap placement and largely restores velopharyngeal competence irrespective of VPI etiology, with low complication rates. Short operative time and LOS extend the value proposition, making this technique not only efficacious but also a resource-efficient option for surgical management of severe VPI.


咽瓣插入软腭穿透解剖:一种“好-快-便宜”的技术,适用于任何病因的腭咽功能不全。
目的:探讨软腭透剥术治疗腭咽功能不全(VPI)的疗效及资源利用。设计:回顾性审查。环境:三级保健中心。患者:纳入30例患者。纳入标准为:经鼻内窥镜或显像透视检查证实,基于感知语音评估诊断为严重VPI;改良咽瓣软腭透剥术治疗VPI;至少6个月的随访。排除22q11.2缺失综合征患者。干预:改良咽瓣与软腭的彻底分离。主要结果测量:使用语言病理学家3级量表评估腭咽能力和语言。结果:术前言语评分中位数为11分(范围7 ~ 13分),术后言语评分中位数为1分(范围0 ~ 7分);P < 0.001)。25例(83%)患者恢复腭咽能力,3例(10%)患者恢复边缘能力,2例(7%)患者持续存在VPI。并发症包括1例需要择期翻修的腭瘘和1例不需要取瓣的轻度阻塞性睡眠呼吸暂停。平均皮对皮手术时间为73.5分钟,平均住院时间(LOS)为50.3小时。结论:该技术可以直接看到皮瓣的位置,并在很大程度上恢复腭咽功能,而不考虑VPI的病因,并发症发生率低。较短的手术时间和LOS扩展了价值主张,使该技术不仅有效,而且是严重VPI手术治疗的资源高效选择。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
自引率
0.00%
发文量
0

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


