Optical coherence tomography angiography indicates subclinical retinal disease in neuromyelitis optica spectrum disorders.
IF 5
Multiple sclerosis (Houndmills, Basingstoke, England)
Pub Date : 2022-04-01
Epub Date: 2021-07-14
DOI:10.1177/13524585211028831
引用次数: 18
Abstract
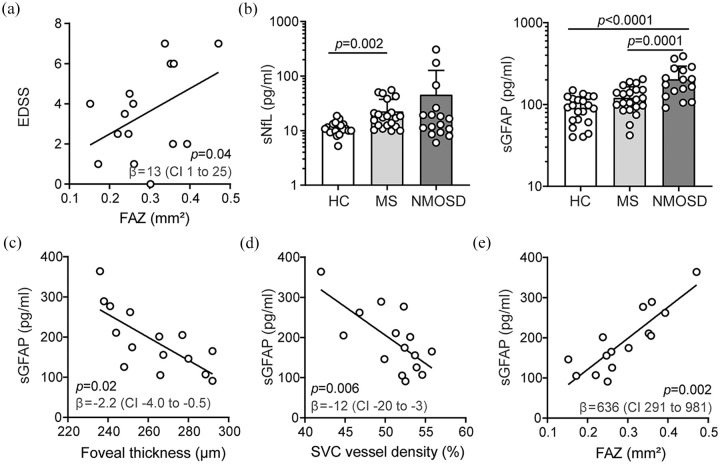
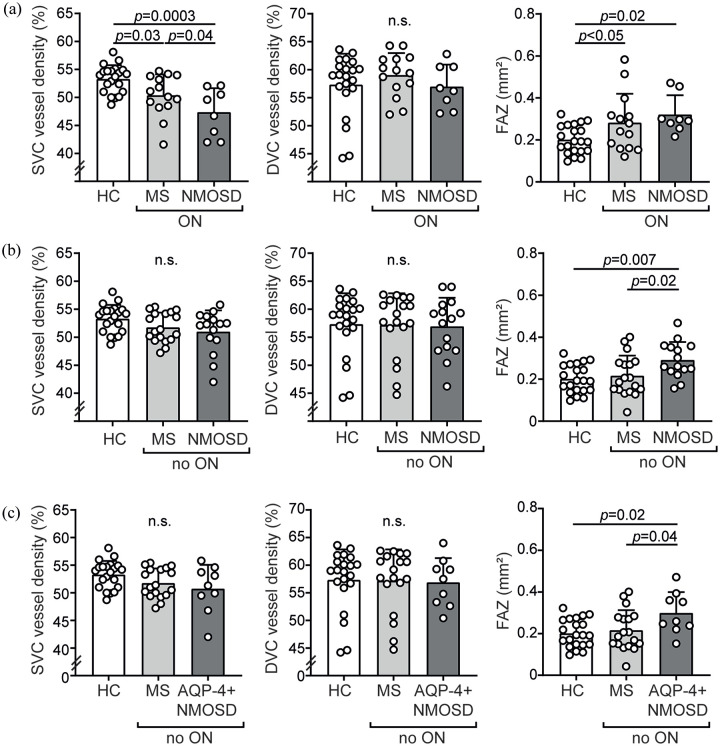
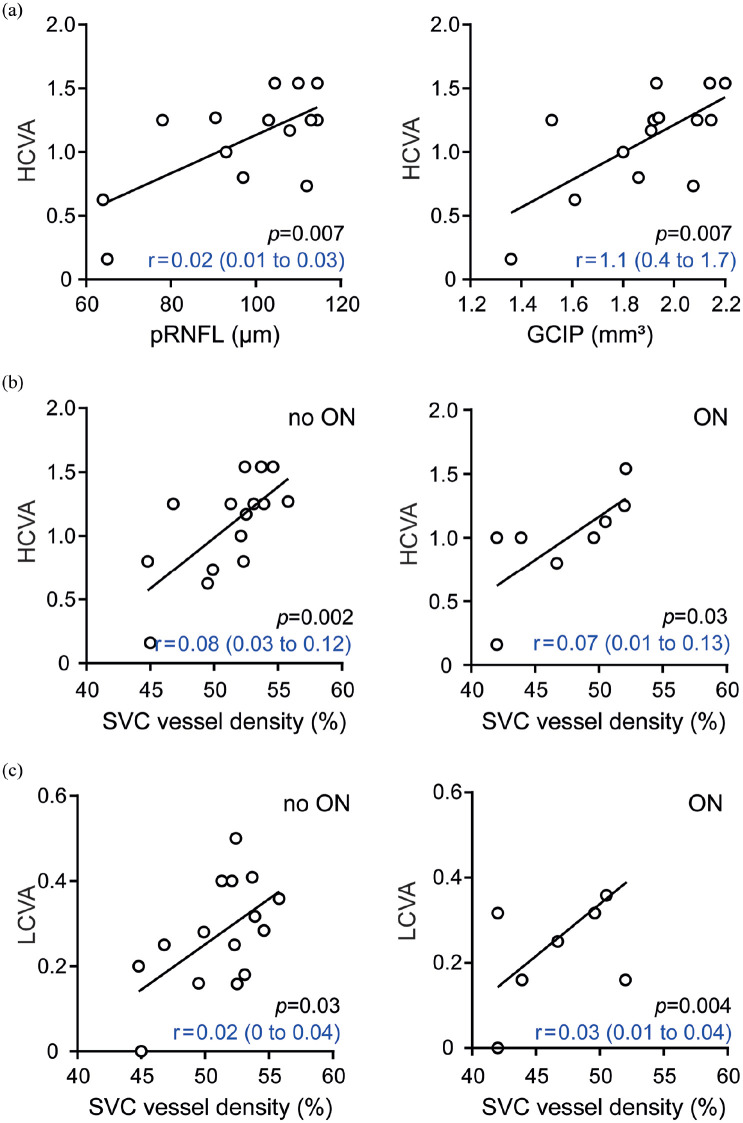
Background: Neuromyelitis optica spectrum disorders (NMOSD) are neuroinflammatory diseases of the central nervous system. Patients suffer from recurring relapses and it is unclear whether relapse-independent disease activity occurs and whether this is of clinical relevance. Objective: To detect disease-specific alterations of the retinal vasculature that reflect disease activity during NMOSD. Methods: Cross-sectional analysis of 16 patients with NMOSD, 21 patients with relapsing-remitting multiple sclerosis, and 21 healthy controls using retinal optical coherence tomography (OCT), optical coherence tomography angiography (OCT-A), measurement of glial fibrillary acidic protein (GFAP) serum levels, and assessment of visual acuity. Results: Patients with NMOSD but not multiple sclerosis revealed lower foveal thickness (FT) (p = 0.02) measures and an increase of the foveal avascular zone (FAZ) (p = 0.02) compared to healthy controls independent to optic neuritis. Reduced FT (p = 0.01), enlarged FAZ areas (p = 0.0001), and vessel loss of the superficial vascular complex (p = 0.01) were linked to higher serum GFAP levels and superficial vessel loss was associated with worse visual performance in patients with NMOSD irrespective of optic neuritis. Conclusion: Subclinical parafoveal retinal vessel loss might occur during NMOSD and might be linked to astrocyte damage and poor visual performance. OCT-A may be a tool to study subclinical disease activity during NMOSD.
光学相干断层扫描血管造影显示亚临床视网膜疾病的神经脊髓炎视谱障碍。
背景:视神经脊髓炎谱系障碍(NMOSD)是中枢神经系统的神经炎性疾病。患者反复复发,目前尚不清楚是否会发生与复发无关的疾病活动,以及这是否与临床相关。目的:检测反映NMOSD期间疾病活动性的视网膜脉管系统的疾病特异性改变。方法:采用视网膜光学相干断层扫描(OCT)、光学相干断层扫描血管造影(OCT- a)、血清胶质纤维酸性蛋白(GFAP)水平测定和视力评估,对16例NMOSD患者、21例复发-缓解型多发性硬化症患者和21例健康对照进行横断面分析。结果:与独立视神经炎的健康对照相比,非多发性硬化症的NMOSD患者的中央凹厚度(FT)较低(p = 0.02),中央凹无血管带(FAZ)增加(p = 0.02)。FT降低(p = 0.01)、FAZ面积增大(p = 0.0001)和浅表血管复合物的血管丢失(p = 0.01)与血清GFAP水平升高有关,而与视神经炎无关,NMOSD患者的浅表血管丢失与视力下降有关。结论:NMOSD可能发生亚临床视网膜中央凹旁血管丢失,可能与星形胶质细胞损伤和视力下降有关。OCT-A可能是研究NMOSD期间亚临床疾病活动的工具。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


