The Role of the Posterolateral Tibial Slope in the Rotational Instability of the Knee in Patients Affected by a Complete Isolated Anterior Cruciate Ligament Injury: Its Value in the Decision-Making Process during the Anterolateral Ligament Reconstruction.
Q1 Medicine
引用次数: 5
Abstract
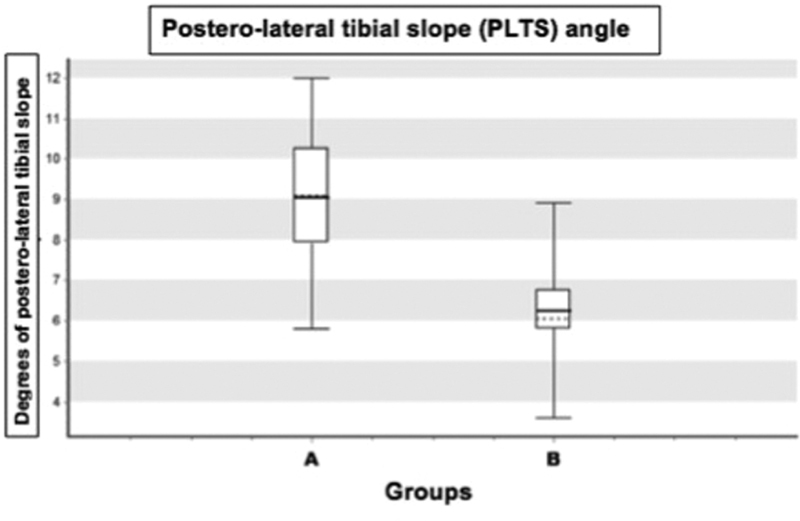
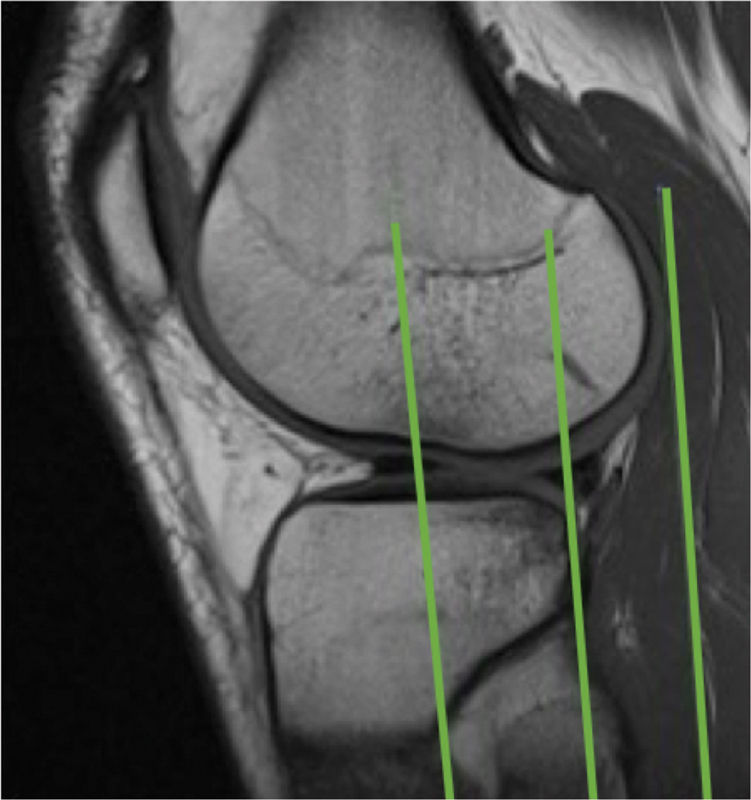
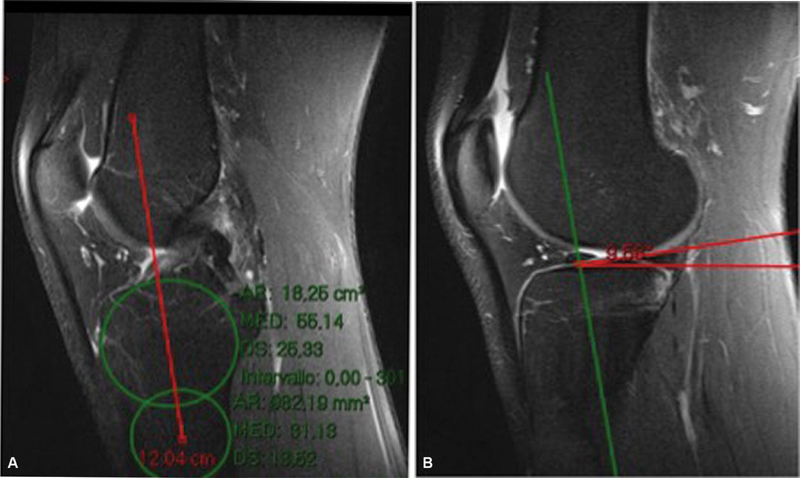
Abstract Purpose The aim of this retrospective, multicenter study was to investigate the correlation between a high degree of rotatory instability, posterolateral tibial slope (PLTS), and anterolateral ligament (ALL) injury. Methods The study population consisted of 76 adults with isolated, complete noncontact anterior cruciate ligament (ACL) tear. The sample was divided into two groups according to the preoperative degree of rotator instability (group A: pivot-shift test grades 2 and 3; group B: pivot-shift test grade 1). Preoperative magnetic resonance imaging (MRI) assessment included angle of PLTS, posterior shift of the lateral femoral condyle (16 mm) on the tibial plateau, and the presence/absence of ALL injury. The two groups were compared for differences. Results There was a statistically significant association between pivot-shift test grades 2 and 3 (group A), PLTS slope angle > 9 degrees, and ALL injury (p < 0.05). Group A also demonstrated a greater posterior shift of lateral femoral condyle (>11 mm), which was, however, not statistically significant when evaluated as an isolated variable. Conclusion Our study indicates that an increased PLTS is associated with an increased incidence of ALL injury and an increased grade of pivot shift in patients with ACL tear. Assessment of posterolateral tibial slope on MRI can therefore play a key adjunct role in the surgical planning of ALL reconstruction, especially in cases when ALL damage is radiologically difficult to detect or doubtful. Level of Evidence This is a retrospective comparative level III study.
胫骨后外侧斜度在完全孤立前交叉韧带损伤患者膝关节旋转不稳定中的作用:其在前外侧韧带重建决策过程中的价值。
目的:本回顾性、多中心研究的目的是探讨高度旋转不稳定性、胫骨后外侧斜度(PLTS)和前外侧韧带(ALL)损伤之间的关系。方法研究对象为76例成人孤立性、完全性非接触性前交叉韧带撕裂。根据术前旋转体不稳定程度将样本分为两组(A组:枢轴移位试验等级2和3;B组:枢轴移位试验1级)。术前磁共振成像(MRI)评估包括PLTS角度、胫骨平台上股骨外侧髁后侧移位(16 mm)以及ALL损伤的存在/缺失。比较两组的差异。结果枢轴移位测试等级2和3 (a组)、PLTS倾斜角度> 9度和ALL损伤(p 11 mm)之间存在统计学意义的关联,但作为孤立变量评估时,这一关联无统计学意义。结论:我们的研究表明,在前交叉韧带撕裂患者中,PLTS增加与ALL损伤发生率增加和枢轴移位程度增加有关。因此,在MRI上评估胫骨后外侧斜度可以在ALL重建的手术计划中发挥关键的辅助作用,特别是在ALL损伤在放射学上难以发现或怀疑的情况下。证据水平这是一项回顾性比较III级研究。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Joints
Medicine-Rehabilitation
CiteScore
4.30
自引率
0.00%
发文量
0
期刊介绍:
Joints is the official publication of SIGASCOT (Italian Society of the Knee, Arthroscopy, Sports Traumatology, Cartilage and Orthopaedic Technology). As an Open Acccess journal, it publishes papers on clinical and basic research, review articles, technical notes, case reports, and editorials about the latest developments in knee surgery, arthroscopy, sports traumatology, cartilage, orthopaedic technology, upper limb, and related rehabilitation. Letters to the Editor and comments on the journal''s content are always welcome.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


