Ambulatory blood pressure monitoring and blood pressure control in patients with coronary artery disease—A randomized controlled trial
Abstract
Background
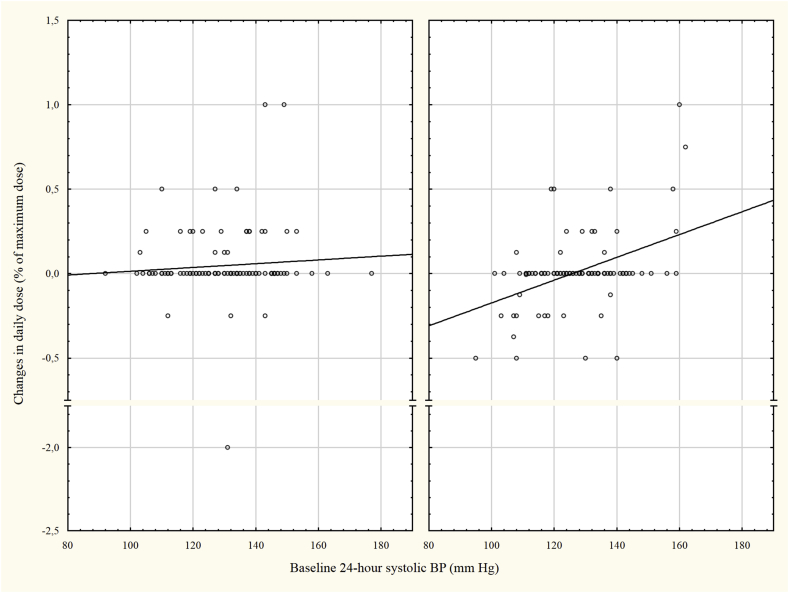
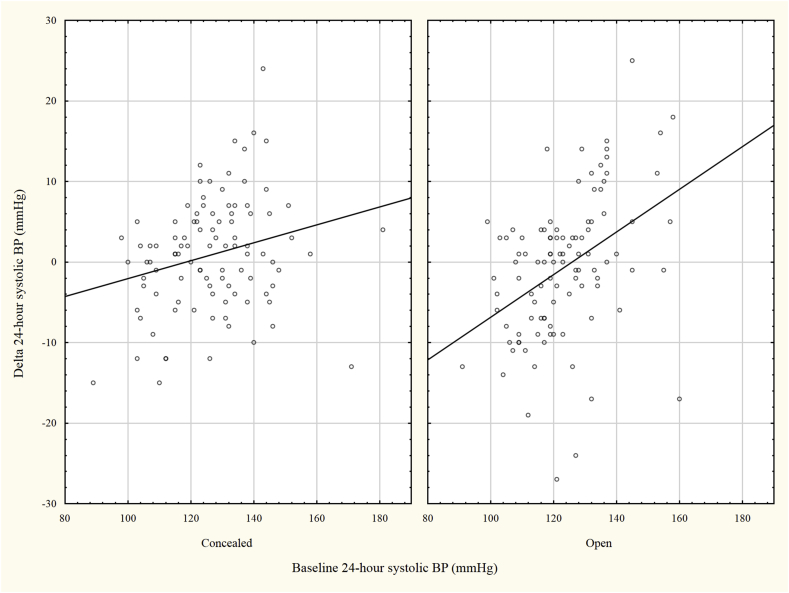
Office blood pressure (OBP) is used for diagnosing and treating hypertension but ambulatory blood pressure measurement (ABPM) associates more accurately with patient outcome. BP control is important in secondary prevention but it is unknown whether the use of APBM improves BP-control in this setting. Our objective was to investigate whether physician awareness of ABP after percutaneous coronary intervention (PCI) improved BP-control. Methods: A total of 200 patients performed ABPM before and after their PCI follow-up visit. Patients were randomized to open (O) or concealed (C) ABPM results for the physician at the follow-up visit. The change in ABP and antihypertensive medication in relation to baseline ABP was compared between the two groups. Results: The average OBP (O and C: 128/76 mmHg) and ABP (O: 123/73 mmHg, C: 127/74 mmHg) was well controlled and did not change between the first and second measurement. A slight increase in systolic ABP during night time was observed in the open arm compared to the concealed arm. Among patients with high ABP (>130/80 mm Hg) at baseline more patients in the C compared to O group remained with a high ABP at the end of study 34/44 (77%) vs 19/34 (56%), p = 0.045. There was a positive correlation between baseline systolic ABP and ABP change in both the O (r = 0.41, p < 0.001) and the C (r = 0.24, p = 0.014) groups but the association was steeper in the open group (p = 0.035). In patients with low ABP an increase and in patients with high ABP a decrease in ABP was observed in the O group where more changes in medication were done. Conclusions: ABPM did not lower blood pressure in patients with CAD apart from in those with elevated ABP but led to more relevant changes in antihypertensive treatments. Further studies are needed to answer whether patient outcome is affected.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


