Central involvement of SARS-CoV-2 may aggravate ARDS and hypertension.
IF 4.1
4区 医学
Q3 PERIPHERAL VASCULAR DISEASE
Journal of the Renin-Angiotensin-Aldosterone System
Pub Date : 2020-10-01
DOI:10.1177/1470320320972015
引用次数: 4
Abstract
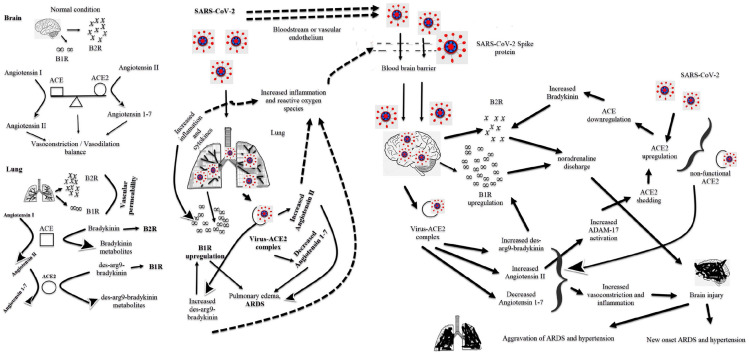
Creative Commons Non Commercial CC BY-NC: This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 License (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage). Dear Sir, Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) continues to spread rapidly all over the world; however, the mechanism of the disease is not yet fully understood. Why do many people who come into contact with the virus not get sick and remain asymptomatic? Why do some people recover with tiny symptoms, while other people have a severe infection or die? SARSCoV-2 infection can lead to severe or fatal outcomes in patients with comorbid diseases such as hypertension, diabetes, obesity, and heart failure. SARS-CoV-2 binds to angiotensin-converting enzyme (ACE)-2, like SARS-CoV, enters the cells and causes infection. The renin-angiotensin system (RAS) plays a crucial role in the virus entry to cells and the progression of the virus-induced disease. Whether ACE2 upregulation will increase viral load remains unclear.1 ACE2 up-regulation increases angiotensin 1–7 formation and may have a protective effect against SARSCOV-2 caused acute respiratory distress syndrome (ARDS) and heart damage.1 Angiotensin II level is high in patients with the novel coronavirus disease 2019 (COVID19). According to an extensive view, SARS-CoV-2 binds to ACE2, causing ACE2 to become dysfunctional.2 Therefore, increased angiotensin II level leads to ARDS and heart damage.2 Interestingly, most infected people have no symptoms, and they do not have heart or lung damage. The effects of SARS-CoV-2 on peripheral RAS have been highlighted so far. We believe that the central RAS involvement of the virus has vital implications for COVID-19 progression. Regulation of pulmonary vascular tone is vital for the maintenance of pulmonary functions. RAS regulates vasoconstriction and vasodilation of the pulmonary vascular system. Bradykinin and kinin are responsible for the permeability and vasodilation of the pulmonary vascular system (Figure 1). Inflammation leads to an increase in bradykinin-1 receptor (B1R) in the lungs. They increase vascular permeability by binding bradykinin to the bradykinin-2 receptor (B2R) and des-arg9-bradykinin binding to the B1R. Increased pulmonary vascular permeability causes pulmonary edema.3,4 SARS-CoV-2 can cause ARDS via the bradykinin pathway in the lung (Figure 1).3,4 The brain is one of the tissues containing ACE2, such as the lung, heart, pancreas, kidney, and vascular endothelium, and SARS-CoV-2 can easily infect the brain.5,6 The virus infects the brain after can cross the blood-brain barrier either by direct transport through the bloodstream or indirectly by binding to the vascular endothelium (Figure 1).7 The virus may cause cerebrovascular disorders, epileptic seizures, and neurodegenerative diseases with central involvement.5,8 Neuroinflammation of SARSCoV-2 can lead to an increased risk of hospital stay and mortality. The virus can cause brain damage through the bradykinin and des-arg9-bradykinin pathway, as in the lung. Bradykinin has two receptors, and the brain and spinal cord have a few numbers of B1R, while many tissues have B2R.9,10 There is also abundant B2R in the brain. Bradykinin is only a substrate for ACE, and it is not a substrate for ACE2.9,10 The mechanism by which bradykinin causes central hypertension through B2R is well known. Especially, bradykinin injection into the lateral ventricle causes severe systemic hypertension through B2R.10–12 It was observed that bradykinin into the brain caused a high increase in central blood pressure in hypertensive rats than in normotensive rats.13 The central or intrathecal bradykinin injection leads to noradrenaline release and sympathoneuronal pathway activation.11 The development of central hypertension through B1R is less well known than B2R. Not bradykinin, des-arg9-bradykinin binds B1R and is a substrate of ACE2. B1R upregulation occurs in patients with hypertension, heart failure, diabetes, and obesity.14 COVID-19 is aggressive and severe in patients with comorbid diseases such as hypertension, diabetes, obesity, Central involvement of SARS-CoV-2 may aggravate ARDS and hypertension

SARS-CoV-2的中枢性受累可能加重急性呼吸窘迫综合征和高血压。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
CiteScore
6.20
自引率
0.00%
发文量
16
审稿时长
6-12 weeks
期刊介绍:
JRAAS is a peer-reviewed, open access journal, serving as a resource for biomedical professionals, primarily with an active interest in the renin-angiotensin-aldosterone system in humans and other mammals. It publishes original research and reviews on the normal and abnormal function of this system and its pharmacology and therapeutics, mostly in a cardiovascular context but including research in all areas where this system is present, including the brain, lungs and gastro-intestinal tract.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


