Time to Treatment Initiation and Survival in Adult Localized High-Grade Bone Sarcoma.
Q2 Medicine
引用次数: 5
Abstract
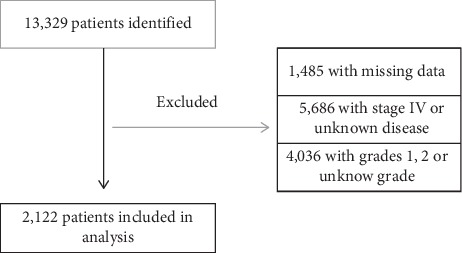
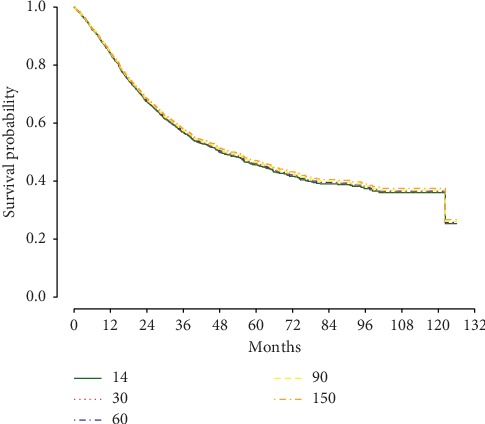
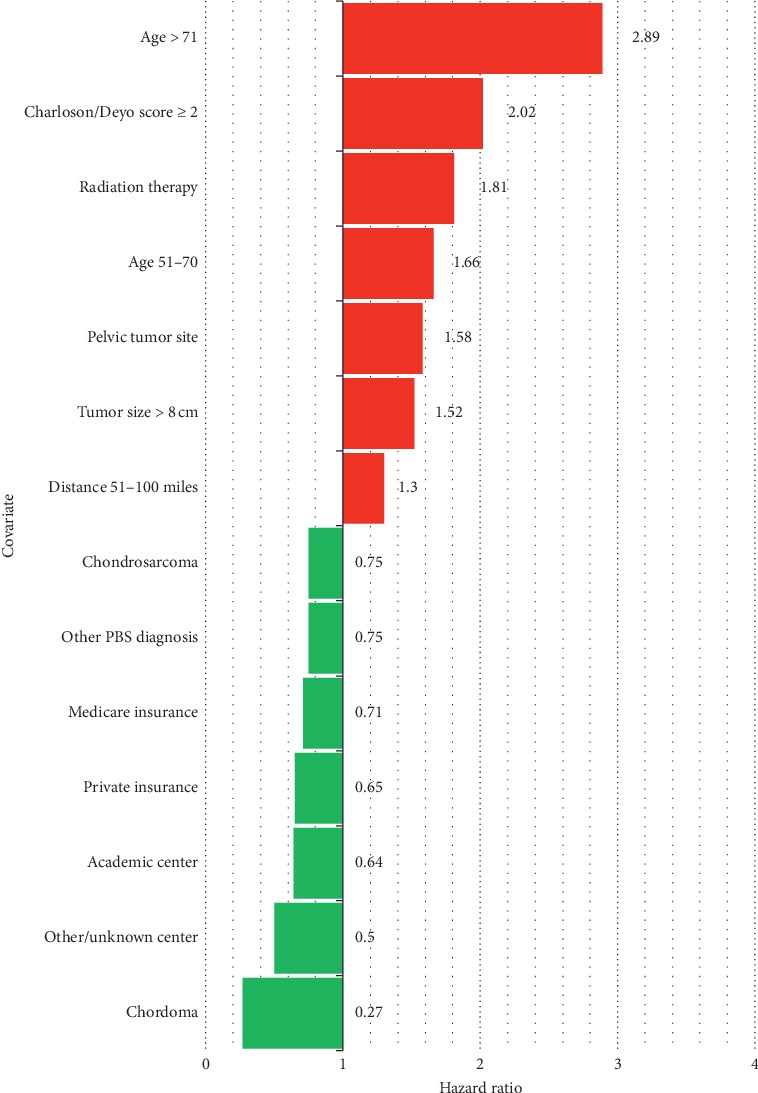
Objective Few studies have evaluated the prognostic implication of the length of time from diagnosis to treatment initiation in bone sarcoma. The purpose of this study is to determine if time to treatment initiation (TTI) influences overall survival in adults diagnosed with primary bone sarcoma. Methods A retrospective analysis of the National Cancer Database identified 2,122 patients who met inclusion criteria with localized, high-grade bone sarcoma diagnosed between 2004 and 2012. TTI was defined as length of time in days from diagnosis to initiation of treatment. Patient, disease-specific, and healthcare-related factors were also assessed for their association with overall survival. Kruskal-Wallis analysis was utilized for univariate analysis, and Cox regression modeling identified covariates associated with overall survival. Results Any 10-day increase in TTI was not associated with decreased overall survival (hazard ratio (HR) = 1.00; P=0.72). No differences in survival were detected at 1 year, 5 years, and 10 years, when comparing patients with TTI = 14, 30, 60, 90, and 150 days. Decreased survival was significantly associated (P < 0.05) with patient ages of 51–70 years (HR = 1.66; P=0.004) and > 71 years (HR = 2.89; P < 0.001), Charlson/Deyo score ≥2 (HR = 2.02; P < 0.001), pelvic tumor site (HR = 1.58; P < 0.001), tumor size >8 cm (HR = 1.52; P < 0.001), radiation (HR = 1.81; P < 0.001) as index treatment, and residing a distance of 51–100 miles from the treatment center (HR = 1.30; P=0.012). Increased survival was significantly associated (P < 0.05) with chordoma (HR = 0.27; P=0.010), chondrosarcoma (HR = 0.75; P=0.002), treatment at an academic center (HR = 0.64; P=0.039), and a private (HR = 0.67; P=0.006) or Medicare (HR = 0.71; P=0.043) insurer. A transition in care was not associated with a survival disadvantage (HR = 0.90; P=0.14). Conclusions Longer TTI was not associated with decreased overall survival in localized, high-grade primary bone sarcoma in adults. This is important in counseling patients, who may delay treatment to receive a second opinion or seek referral to a higher volume sarcoma center.
成人局部高级别骨肉瘤的开始治疗时间和生存率。
目的:很少有研究评估骨肉瘤从诊断到开始治疗的时间长度对预后的影响。本研究的目的是确定治疗起始时间(TTI)是否影响原发性骨肉瘤成人患者的总生存率。方法:对国家癌症数据库进行回顾性分析,确定了2004年至2012年间诊断为局部高级别骨肉瘤的2122例符合纳入标准的患者。TTI定义为从诊断到开始治疗的时间长度(以天为单位)。还评估了患者、疾病特异性和医疗保健相关因素与总生存率的相关性。采用Kruskal-Wallis分析进行单因素分析,Cox回归模型确定与总生存率相关的协变量。结果:任何10天TTI的增加与总生存期的降低无关(风险比(HR) = 1.00;P = 0.72)。与TTI = 14、30、60、90和150天的患者相比,1年、5年和10年的生存率没有差异。患者年龄在51 ~ 70岁之间,生存率降低与患者年龄相关(HR = 1.66;P=0.004)和> 71岁(HR = 2.89;P < 0.001), Charlson/Deyo评分≥2 (HR = 2.02;P < 0.001),盆腔肿瘤部位(HR = 1.58;P < 0.001),肿瘤大小>8 cm (HR = 1.52;P < 0.001),辐射(HR = 1.81;P < 0.001)作为指标治疗,居住距离治疗中心51-100英里(HR = 1.30;P = 0.012)。脊索瘤患者生存率增高(P < 0.05)显著相关(HR = 0.27;P=0.010),软骨肉瘤(HR = 0.75;P=0.002),在学术中心治疗(HR = 0.64;P=0.039),私人(HR = 0.67;P=0.006)或医疗保险(HR = 0.71;P = 0.043)。护理的转变与生存劣势无关(HR = 0.90;P = 0.14)。结论:较长的TTI与成人局部高级别原发性骨肉瘤的总生存率降低无关。这是重要的咨询患者,谁可能会延迟治疗接受第二意见或寻求转诊到更大容量的肉瘤中心。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Sarcoma
Medicine-Radiology, Nuclear Medicine and Imaging
CiteScore
5.00
自引率
0.00%
发文量
15
审稿时长
14 weeks
期刊介绍:
Sarcoma is dedicated to publishing papers covering all aspects of connective tissue oncology research. It brings together work from scientists and clinicians carrying out a broad range of research in this field, including the basic sciences, molecular biology and pathology and the clinical sciences of epidemiology, surgery, radiotherapy and chemotherapy. High-quality papers concerning the entire range of bone and soft tissue sarcomas in both adults and children, including Kaposi"s sarcoma, are published as well as preclinical and animal studies. This journal provides a central forum for the description of advances in diagnosis, assessment and treatment of this rarely seen, but often mismanaged, group of patients.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


