Establishment of Humanized Mice from Peripheral Blood Mononuclear Cells or Cord Blood CD34+ Hematopoietic Stem Cells for Immune-Oncology Studies Evaluating New Therapeutic Agents
Q2 Pharmacology, Toxicology and Pharmaceutics
引用次数: 23
Abstract
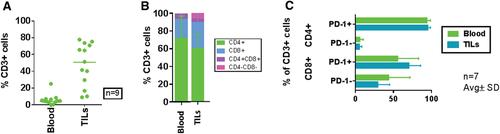
The clinical success of immune checkpoint modulators and the development of next‐generation immune‐oncology (IO) agents underscore the need for robust preclinical models to evaluate novel IO therapeutics. Human immune system (HIS) mouse models enable in vivo studies in the context of the HIS via a human tumor. The immunodeficient mouse strains NOG (Prkdcscid Il2rgtm1Sug) and triple‐transgenic NOG‐EXL [Prkdcscid Il2rgtm1Sug Tg (SV40/HTLV‐IL3, CSF2)], which expresses human IL‐3 and GM‐CSF, allow for human CD34+ hematopoietic stem cell (huCD34+ HSC) engraftment and multilineage immune cell development by 12 to 16 weeks post‐transplant and facilitate studies of immunomodulatory agents. A more rapid model of human immune engraftment utilizes peripheral blood mononuclear cells (PBMCs) transplanted into immunodeficient murine hosts, permitting T‐cell engraftment within 2 to 3 weeks without outgrowth of other human immune cells. The PBMC‐HIS model can be limited due to onset of xenogeneic graft‐versus‐host disease (xGVHD) within 3 to 5 weeks post‐implantation. Host deficiency in MHC class I, as occurs in beta‐2 microglobulin knockout in either NOG or NSG mice, results in resistance to xGVHD, which permits a longer therapeutic window. In this article, detailed processes for generating humanized mice by transplantation of HSCs from cord blood–derived huCD34+ HSCs or PBMCs into immunodeficient mouse strains to respectively generate HSC‐HIS and PBMC‐HIS mouse models are provided. In addition, the co‐engraftment and growth kinetics of patient‐derived and cell line–derived xenograft tumors in humanized mice and recovery of tumor‐infiltrating lymphocytes from growing tumors to evaluate immune cell subsets by flow cytometry are described. © 2020 The Authors.
外周血单核细胞或脐带血CD34+造血干细胞人源化小鼠免疫肿瘤研究及新治疗剂评价
免疫检查点调节剂的临床成功和下一代免疫肿瘤学(IO)药物的发展强调了建立健全的临床前模型来评估新的IO治疗方法的必要性。人类免疫系统(HIS)小鼠模型能够通过人类肿瘤在HIS的背景下进行体内研究。免疫缺陷小鼠品系NOG (Prkdcscid Il2rgtm1Sug)和表达人IL-3和GM-CSF的三转基因NOG- exl [Prkdcscid Il2rgtm1Sug Tg (SV40/HTLV-IL3, CSF2)]可在移植后12 ~ 16周植入人CD34+造血干细胞(huCD34+ HSC)并形成多系免疫细胞,促进免疫调节剂的研究。一种更快速的人类免疫植入模型利用外周血单核细胞(PBMCs)移植到免疫缺陷小鼠宿主中,允许t细胞在2至3周内植入,而不会产生其他人类免疫细胞。由于移植后3 - 5周内发生异种移植物抗宿主病(xGVHD), pmc - his模型可能受到限制。宿主MHC I类缺乏,如在NOG或NSG小鼠中β -2微球蛋白敲除中发生的那样,导致对xGVHD的抵抗,从而允许更长的治疗窗口期。本文详细介绍了将脐带血来源的huCD34+造血干细胞或pbmc移植到免疫缺陷小鼠品系中,分别生成HSC-HIS和PBMC-HIS小鼠模型,生成人源化小鼠的过程。此外,本文还描述了患者来源和细胞系来源的异种移植肿瘤在人源化小鼠体内的共植入和生长动力学,以及肿瘤浸润淋巴细胞在生长肿瘤中的恢复情况,并通过流式细胞术评估免疫细胞亚群。©2020作者。基本方案1:在CD34+造血干细胞人源化小鼠中建立患者源性异种移植肿瘤基本方案2:在外周血单核细胞人源化小鼠中建立患者源性异种移植肿瘤支持方案1:小鼠人源化的流式细胞术评估支持方案2:荷瘤人源化小鼠模型中肿瘤浸润淋巴细胞的流式细胞术评估
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Current Protocols in Pharmacology
Pharmacology, Toxicology and Pharmaceutics-Pharmacology
自引率
0.00%
发文量
0
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


