Jellyfish Stings Rarely Induced Infectious Cellulitis: First Aid Remedies as Double-Edged Sword.
Advanced Journal of Emergency Medicine
Pub Date : 2019-09-29
eCollection Date: 2020-01-01
DOI:10.22114/ajem.v0i0.260
引用次数: 1
Abstract
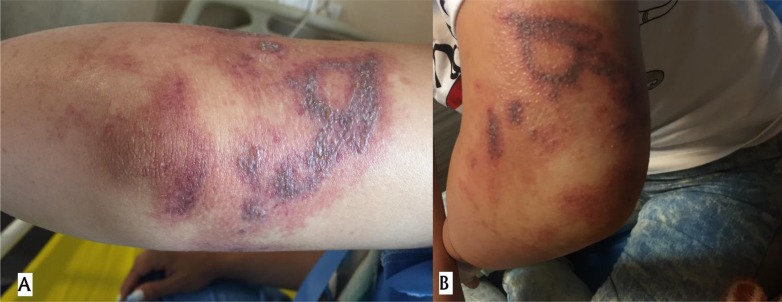
A 27-year-old woman was presented with a burning like lesion. The skin lesion was developed after a jellyfish stings (Rhizostomae) while she was swimming in Pattaya Sea in Thailand, five days prior to her presentation. Instantly after jellyfish stings, she was taken into the ship for rescue operations. The ship personnel applied lemon juice and baking soda to the injured area believing that this remedy is efficient in this situation. The next day, she referred to a local hospital at Pattaya because she was suffering from a horrible pain in her arm and then she was discharged on oral Dicloxacillin and topical Hydrocortisone. The edema was extended the next days which intensified her pain. At this time, she was transferred to Loghman Hakim Hospital, Tehran, Iran. At admission, erythematous edematous patch with centrally grouped vesicles on the left arm was observed (Figure 1). The patient had a high-grade fever (38.1 °C) and was agitated due to her intolerable pain. Other vital signs were normal. In the sonography imaging, soft tissue edema was seen without any collection. According to the clinical and imaging findings, the diagnosis of soft tissue cellulitis due to jellyfish stings was made. The patient admitted to infections ward and intravenous antibiotics including Cefazolin at dose of 2000 mg every eight hours and Vancomycin at dose of 1000 mg every 12 hours initiated. After five days of hospitalization, the patient was recovered from left arm edema. Also, her pain decreased gradually and no obvious erythema was seen. The patient was finally discharged with a satisfactory clinical response
水母蜇伤很少引起感染性蜂窝织炎:急救措施是一把双刃剑。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


