Is this a satellite orbiting unchartered territory?
IF 3.2
Q2 CARDIAC & CARDIOVASCULAR SYSTEMS
Echo Research and Practice
Pub Date : 2020-02-17
eCollection Date: 2020-03-01
DOI:10.1530/ERP-19-0061
引用次数: 0
Abstract
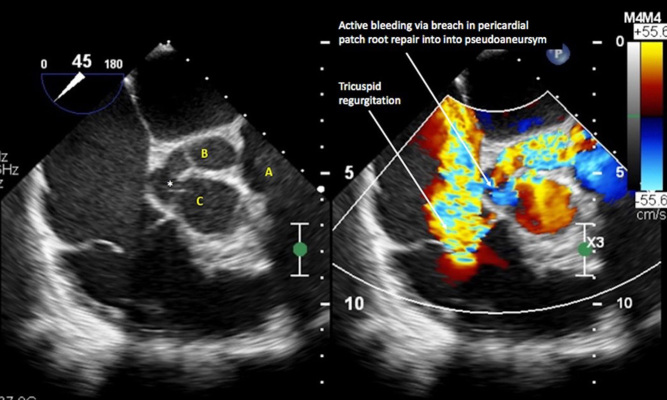
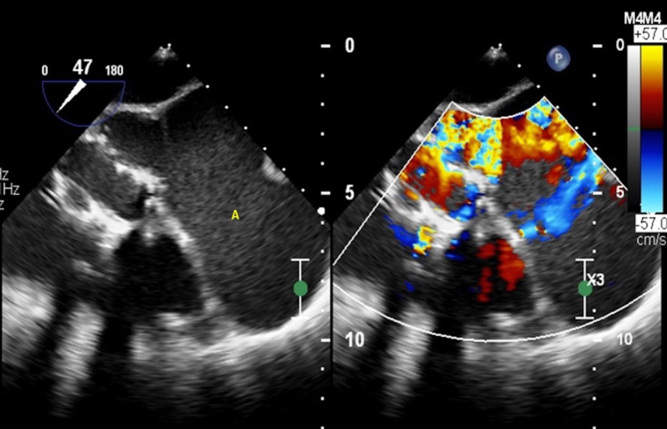
A 27-year old female i.v. drug user presented to our institution with chest pain. She had a history of bicuspid aortic valve endocarditis with aortic root abscess repaired with bioprosthetic aortic valve replacement and pericardial patch reconstruction of the left ventricular outflow tract and non-coronary sinus 6 weeks previously. Echocardiographic and cardiac CT imaging confirmed three foci of breakdown of the pericardial patch repair with active bleeding into a large posterior pseudoaneurysm (92 mm diameter) compressing the left atrium and pulmonary artery. Following multidisciplinary discussion, the consensus was to attempt urgent percutaneous closure of the defect, given the prohibitive surgical risks. The procedure was performed under fluoroscopic and 3D-transoesophageal guidance. TOE demonstrated the pericardial patch breaches and active bleeding into the large pseudoaneurysm (Figs 1 and 2). Initial deployment of an Amplatzer atrial septal defect occluder resulted in significant flow reduction, but there remained two small peri-device leaks (Fig. 3). During an attempt to implant an additional smaller Amplatzer vascular plug (AVP-2) to rectify this, the initial device dislodged and embolised into the pseudoaneurysm. This was felt irretrievable and unlikely to be clinically significant given its containment. The embolised device freely floated within the pseudoaneurysm, uniquely akin to a satellite orbiting in space (Video 1). The secondary device was removed and initial breach was satisfactorily closed with a 15-mm-sized Amplatzer atrial septal defect occluder (third device). This was confirmed to be wellseated on real-time 3D imaging (Video 2), with negligible residual leak on TOE (Fig. 4). This is the first published case of percutaneous cardiac device embolization into a pseudoaneurysm cavity that we are aware of. ID: XX-XXXX;

这是一颗绕未知区域运行的卫星吗?
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Echo Research and Practice
CARDIAC & CARDIOVASCULAR SYSTEMS-
CiteScore
6.70
自引率
12.70%
发文量
11
审稿时长
8 weeks
期刊介绍:
Echo Research and Practice aims to be the premier international journal for physicians, sonographers, nurses and other allied health professionals practising echocardiography and other cardiac imaging modalities. This open-access journal publishes quality clinical and basic research, reviews, videos, education materials and selected high-interest case reports and videos across all echocardiography modalities and disciplines, including paediatrics, anaesthetics, general practice, acute medicine and intensive care. Multi-modality studies primarily featuring the use of cardiac ultrasound in clinical practice, in association with Cardiac Computed Tomography, Cardiovascular Magnetic Resonance or Nuclear Cardiology are of interest. Topics include, but are not limited to: 2D echocardiography 3D echocardiography Comparative imaging techniques – CCT, CMR and Nuclear Cardiology Congenital heart disease, including foetal echocardiography Contrast echocardiography Critical care echocardiography Deformation imaging Doppler echocardiography Interventional echocardiography Intracardiac echocardiography Intraoperative echocardiography Prosthetic valves Stress echocardiography Technical innovations Transoesophageal echocardiography Valve disease.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


