Successful Femtosecond Laser-assisted Cataract Surgery for a Cataract with Persistent Pupillary Membrane: A Case Report.
Q3 Medicine
Korean Journal of Ophthalmology : KJO
Pub Date : 2022-10-01
Epub Date: 2022-10-04
DOI:10.3341/kjo.2022.0046
引用次数: 0
Abstract
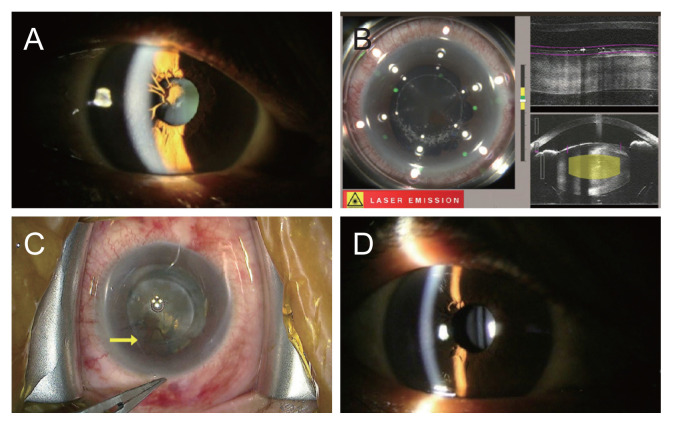
Dear Editor, The persistent pupillary membrane (PPM) is a remnant of the tunica vasculosa lentis, which provides blood supply for fetal crystalline lens development. During normal fetal development, the tunica vasculosa lentis undergoes involution and disappears between the 8th and 9th gestational months. The PPM develops due to incomplete atrophy of the fetal pupillary membrane [1]. Rarely, if a thick PPM covers the visual axis, administration of topical atropine or surgical intervention is required to prevent the progression of amblyopia and improve visual acuity [1]. Previous studies have reported on the surgical excision of a remnant membrane with cataract surgery or neodymium-doped yttrium aluminum garnet (Nd-YAG) laser lysis of the PPM before phacoemulsification [2,3]. Femtosecond laser-assisted cataract surgery (FLACS), which includes three main steps (corneal arcuate incision, anterior capsulotomy, and lens fragmentation), is an advanced technology that increases the accuracy and reduces the complications compared to conventional cataract surgery [4]. The advantages of FLACS include astigmatism correction, increased stability of the implanted intraocular lens with reproducibility and accuracy of capsulotomy, and reduced use of ultrasound [4]. Capsulotomy performed using the femtosecond laser can excise the PPM, reduce the risk of intraoperative bleeding, and help ensure visibility of the surgical field [5]. Here, we report a case in which a cataract in an eye with a PPM was treated by FLACS. Written informed consent for publication of this case and clinical images was obtained from the patient. A 61-year-old female patient presented to the ophthalmology department of Severance Hospital with bilateral decreased visual acuity and visual discomfort. She had diabetes mellitus but had no history of ocular trauma or operation and no familial ocular disease. Her preoperative corrected distant visual acuity (CDVA) was 0.3 (decimal) with autorefraction -3.00 diopters (D) -1.50 D × 138° in the right eye and 0.7 (decimal) with +2.25 D -0.75 D × 84° in the left eye. The intraocular pressure was 17 and 18mmHg in the right and left eyes, respectively, using a noncontact tonometer. On slit-lamp examination, we observed cataracts with nuclear opacity grade 3 by Lens Opacities Classification System III classification in her both eyes and PPM in her right eye. The pupillary threads were superotemporally connected to the other parts of the iris and attached to the anterior lens capsule (Fig. 1A). Although the PPM did not completely cover the pupil, it was suspected to adversely affect her visual acuity with the cataract in the right eye. The patient was scheduled to undergo FLACS in both eyes, with an interval of 1 week between the left and right eye. We used a LenSx femtosecond laser system (Alcon, Aliso Viejo, CA, USA). Most of the PPM strands were disconnected during the anterior capsulotomy step using the femtosecond laser (Fig. 1B, 1C). However, anterior capsulotomy was suspected to be incomplete on the side of the thick strands. The capsulotomy was completed by holding the edge of the anterior capsule using capsulorhexis forceps and pulling it carefully toward the center of the lens. The cut PPM and anterior capsule were successfully removed together, and the remaining surgical procedures were completed without any problems. The postoperative follow-up showed a perfectly round pupil with removed PPM and an adequately positioned intraocular lens in the bag (Fig. 1D). The patient revealed a stable course without complications like intraocular pressure elevation, infection, and macular edema. At the 1-month postoperative follow-up, her CDVA was 1.0 (decimal) in both eyes with manifest refraction -0.25 D × 90° in the right eye and -0.50 D in the left eye, respectively. This case shows that PPM can be removed concurrently with cataract surgery using a femtosecond laser, without Korean J Ophthalmol 2022;36(5):474-475 https://doi.org/10.3341/kjo.2022.0046
飞秒激光辅助白内障手术成功治疗持续性瞳孔膜白内障1例。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


