The prognostic impact of perioperative blood transfusion on survival in patients with bladder urothelial carcinoma treated with radical cystectomy.
引用次数: 20
Abstract
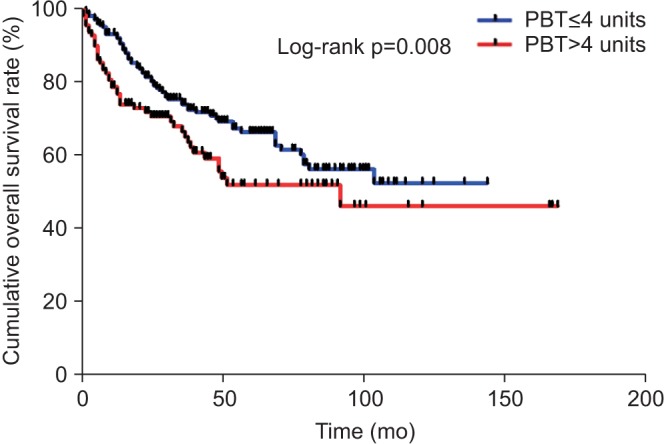
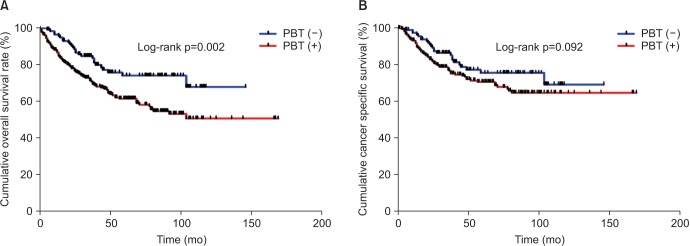
PURPOSE The aim of our study was to assess the influence of perioperative blood transfusion (PBT) on survival outcomes following radical cystectomy (RC) and pelvic lymph node dissection (PLND). MATERIALS AND METHODS We reviewed and analyzed the clinical data of 432 patients who underwent RC for bladder cancer from 1991 to 2012. PBT was defined as the transfusion of allogeneic red blood cells during RC or postoperative hospitalization. RESULTS Of all patients, 315 patients (72.9%) received PBT. On multivariate logistic regression analysis, female gender (p=0.015), a lower preoperative hemoglobin level (p=0.003), estimated blood loss>800 mL (p<0.001), and performance of neoadjuvant chemotherapy (p<0.001) were independent risk factors related to requiring perioperative transfusions. The receipt of PBT was associated with increased overall mortality (hazard ratio, 1.91; 95% confidence interval, 1.25-2.94; p=0.003) on univariate analysis, but its association was not confirmed by multivariate analysis (p=0.058). In transfused patients, a transfusion of >4 packed red blood cell units was an independent predictor of overall survival (p=0.007), but not in cancer specific survival. CONCLUSIONS Our study was not conclusive to detect a clear association between PBT and survival after RC. However, the efforts should be made to continue limiting the overuse of transfusion especially in patients who are expected to have a high probability of PBT, such as females and those with a low preoperative hemoglobin level and history of neoadjuvant chemotherapy.

膀胱尿路上皮癌根治性膀胱切除术患者围手术期输血对生存的影响。
目的:本研究的目的是评估围手术期输血(PBT)对根治性膀胱切除术(RC)和盆腔淋巴结清扫(PLND)后生存结果的影响。材料与方法:回顾分析1991年至2012年432例膀胱癌行RC的临床资料。PBT被定义为在RC或术后住院期间输注异体红细胞。结果:315例(72.9%)患者接受了PBT治疗。在多因素logistic回归分析中,女性(p=0.015)、较低的术前血红蛋白水平(p=0.003)、估计失血量>800 mL (p4填充红细胞单位)是总生存率的独立预测因子(p=0.007),但不是癌症特异性生存率的独立预测因子。结论:我们的研究并不能确定PBT与RC后生存之间的明确联系。然而,应继续努力限制输血的过度使用,特别是在预计PBT的高概率患者中,如女性和术前血红蛋白水平低和新辅助化疗史的患者。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


