Entrustable professional activities - visualization of competencies in postgraduate training. Position paper of the Committee on Postgraduate Medical Training of the German Society for Medical Education (GMA).
GMS Zeitschrift fur Medizinische Ausbildung
Pub Date : 2013-11-15
eCollection Date: 2013-01-01
DOI:10.3205/zma000890
引用次数: 44
Abstract
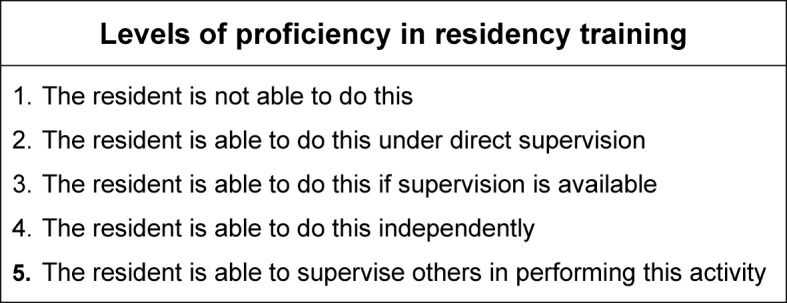
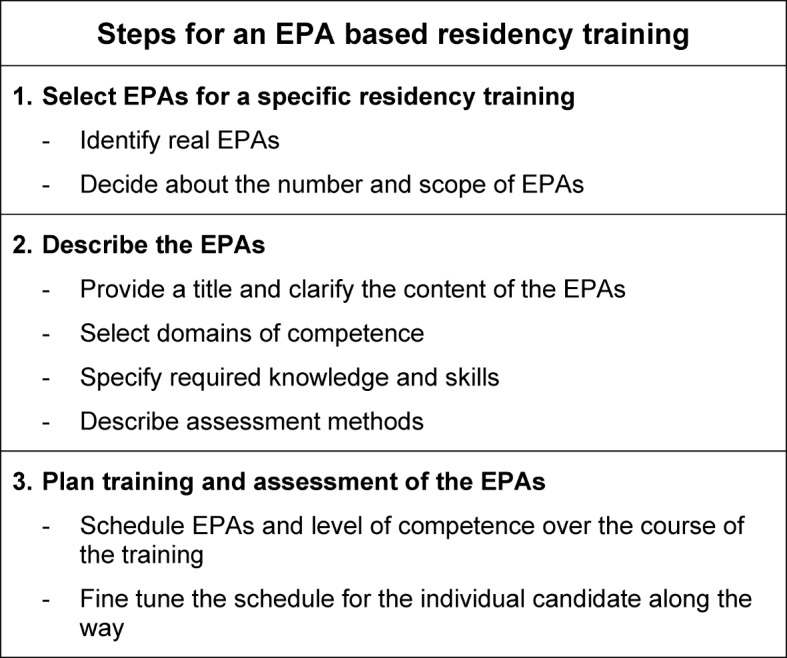
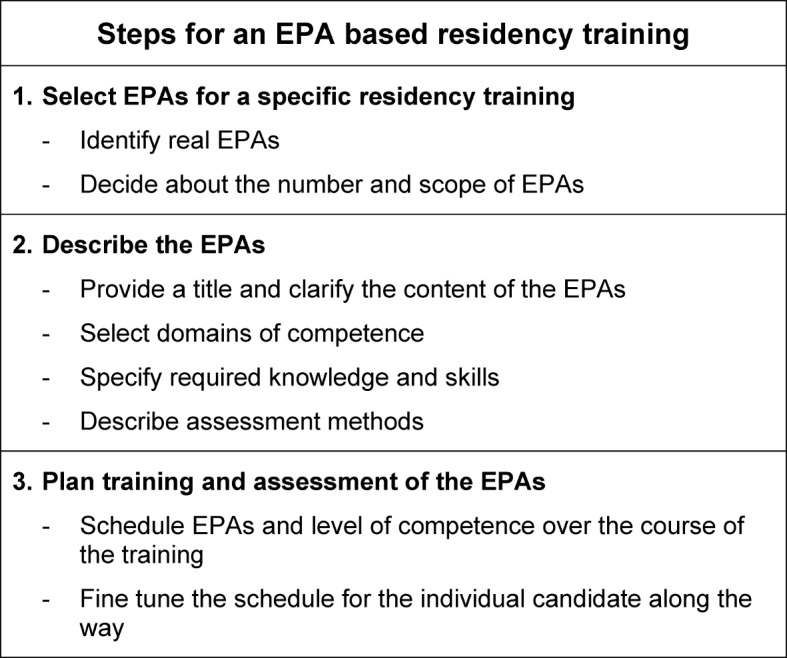
Quality and structure of postgraduate medical training and educational experiences in undergraduate and postgraduate training play a major role in career decisions of young medical graduates [14], [19], [23], [28]. They consider structured mandatory and challenging postgraduate training programmes delivered by experienced trainers with high training competencies as important factors of attractiveness and good starting of their clinical career [23]. The present postgraduate training in Germany widely differs between the medical disciplines. Best-practice examples of a structured competency-based postgraduate training that may serve as models for other clinical fields exist for anaesthesiology [24], family medicine [25], urology [11] and surgery [18]. However, a national comprehensive and binding curricular structure ensuring comparable competencies independent of training site is missing. Certification examinations in all medical disciplines follow an unstructured oral assessment format outside of the clinical context. Thus, it neither adequately assesses clinical competencies of medical doctors at the time of certification nor does it represent professional tasks [Musterweiterbildungsordnung 2003 der Bundesarztekammer (accessed February 12, 2013)]. The evaluation of postgraduate training launched by the German Medical Association in 2009 and 2011 revealed mediocre overall satisfaction of the trainees [Bundesrapport 2009. Evaluation der Weiterbildung in Deutschland (accessed February 12, 2013)], [Bundesrapport 2011. Evaluation der Weiterbildung in Deutschland (accessed February 12, 2013)]. Forty-five percent of the respondents rated postgraduate training between satisfactory and failed on a school grade scale. More than a third evaluated the training culture in their work environment and the support in acquiring professional competencies as only satisfactory to deficient. The most worrying result was the lack of training in evidence-based medicine and its transfer to the delivery of patient care, which 69% of respondents rated as only satisfactory or below. As for transparency of postgraduate training, only one third of the respondents obtained a structured plan and defined outcome objectives in written form, 42% received no training schedule at all [Bundesrapport 2011. Evaluation der Weiterbildung in Deutschland (accessed February 12, 2013)]. There was a slight improvement between the two evaluation cycles in 2009 and 2011 suggesting the necessity of a further decisive and perceptible action plan to advance the present postgraduate training culture in Germany. Currently, a vigorous discussion on the future of postgraduate medical training in Germany is ongoing among political stakeholders, the German Medical Association, the State Chambers of Physicians, scientific medical societies, professional medical organizations and all physicians in charge of postgraduate training supervision. On the 115th annual conference of the German Physicians Board 2012 the managing-committee of the German Medical Association was requested to work out concrete propositions for new Postgraduate Professional Education Regulations, which represent the reality of health care provision today and define professional competencies as essential outcomes of postgraduate training [15]. The suggestion to entirely omit guiding numerical values for medical procedures in favour of competencies was not supported by the majority. However, there is agreement that the new regulations should include the following fundamentals: Definition of competency-based educational goals, integration of domains and levels of competencies, a focus on educational contents rather than duration, a reduction of numerical values for medical procedures [Bartmann F-J. Musterweiterbildungsordnung – Sachstand zur Novellierung. 2013 (accessed June 29, 2013)]. In order to facilitate an exchange of ideas the German Medical Association has established the "WIKI-BAK-Platform" in December 2012 to allow scientific medical societies and professional medical organizations to place their propositions and thus contribute to the new regulations for certification between February and April 2013 [Bundesarztekammer (accessed February 12, 2013)]. In Austria the present situation in postgraduate medical training appears similar to that in Germany: evaluation reveals only mediocre overall satisfaction of the trainees. There is an ongoing discussion, based on the reform of undergraduate training in 2002 and the increased mobility of young doctors, that postgraduate training urgently needs new and more structured curricula. They should pursue the agreed and planned competency-based education of the final year of undergraduate training and follow a modular structure with internship, common trunk and major/elective subjects. A slightly different situation is reported form Switzerland: all postgraduate training programs were accredited in 2011, and the national postgraduate training regulation was revised in 2013. An independent institute, the Swiss Institute for Postgraduate Training (SIWF), is responsible. Regarding the orientation towards professional competencies as outcomes of postgraduate training the present national regulation defines general outcomes for all programs. These are listed in detail in an associated catalogue of general learning objectives based on the CanMEDS roles and integrating other frameworks like the ACGME General Competencies [Lernzielkatalog – Allgemeine Lernziele fur die Weiterbildungsprogramme (accessed October 19, 2013)]. Moreover different postgraduate training programs have implemented workplace-based assessments aiming at monitoring the achievement of professional competencies [20]. The present situation represents an ideal chance for considering and implementing new concepts of postgraduate training which would stress the continuum of undergraduate and postgraduate training as well as continuous professional development [17]. The Society for Medical Education (GMA) should have a significant share in the discussion and promotion of the ongoing process of developing an interdisciplinary evidence-based postgraduate education strategy for Germany in the 21st century. The Committee on Postgraduate Medical Education of the GMA has elucidated crucial questions and formulated essential stimuli supporting the current process [4]. This position paper is aimed at presenting successful competency-based frameworks for postgraduate medical education and appreciating prospects of integrating these frameworks in the current German reforms.
可信赖的专业活动——研究生培养能力的可视化。德国医学教育协会研究生医学培训委员会的立场文件。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


