Are we misleading users of respiratory spacer devices?
引用次数: 3
Abstract
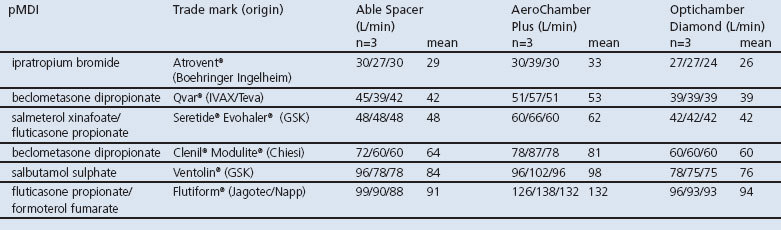
VHC whistles would be activated if the patient goes beyond a flow rate of 60 L/min (the top end of the ideal inspiratory flow rate). However, our research with three whistle-containing VHCs suggests that this appears to be an erroneous assumption and, unwittingly, we may be misleading patients and therefore contributing to reduced patient care. We measured the whistle-activation flow rates for three different makes of VHCs: Able Spacer (Clement Clarke), AeroChamber Plus (GSK), and Optichamber Diamond (Philips Respironics). A calibrated waveform generator (Pulmonary Waveform Generator System, MH Custom Design & Mfg L.C., Utah, USA) was used to create a standardised vacuum force similar to a human inhalation. The performance of three samples of each device was assessed when used with a range of popular drug pMDIs (see Table). The vacuum force was repeated at 1 L/min incremental amounts until the VHCwhistle sounded. Two operatives agreed the whistle sounding. Three recordings of each VHC-drug pMDI combination were carried out (n=54 tests) and the flow rates recorded. The data show that there is a wide variation in the performance of a VHC-whistle as a function of the inhaler to which it is attached. In many instances the whistle first activates at a flow rate well beyond what would be considered acceptable in order to promote effective drug deposition. This phenomenon can be explained. When the patient inhales from the VHC, air will be drawn in through a combination of two routes – the whistle, and the channels surrounding the canister of Dear Sirs, The UK Drug Tariff lists a number of spacer and valved holding chamber (VHC) products for use with pressurised metered dose inhalers (pMDIs). These add-on devices have the double objective of improving the delivery of drug, and making the inhalation procedure easier for the patient. VHCs, in particular, help the user by eliminating the requirement that the slow deep inspiration coincides with the actuation of the pMDI – a manoeuvre which can be particularly tricky for children and the elderly, although poor coordination is worryingly common in pMDI users irrespective of age. VHC users should inhale gently, using either tidal breathing or an approximate 30 L/min inspiratory flow, which facilitates lung deposition of the drug particles. Some VHC products include an alert whistle designed to sound “when the patient is breathing in too quickly”, as this type of forceful inspiratory manoeuvre increases the likelihood of oral/pharyngeal drug deposition. It is known that healthcare trainers use the whistle-alert as a tool to titrate the Prim Care Respir J 2013; 22(4): 466-467
我们是否在误导呼吸间隔器的使用者?
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Primary Care Respiratory Journal
PRIMARY HEALTH CARE-RESPIRATORY SYSTEM
自引率
0.00%
发文量
0
审稿时长
6-12 weeks
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


