Extramedullary blast crisis of secondary CML accompanying marrow fibrosis.
The Korean Journal of Hematology
Pub Date : 2012-12-01
Epub Date: 2012-12-24
DOI:10.5045/kjh.2012.47.4.243
引用次数: 3
Abstract
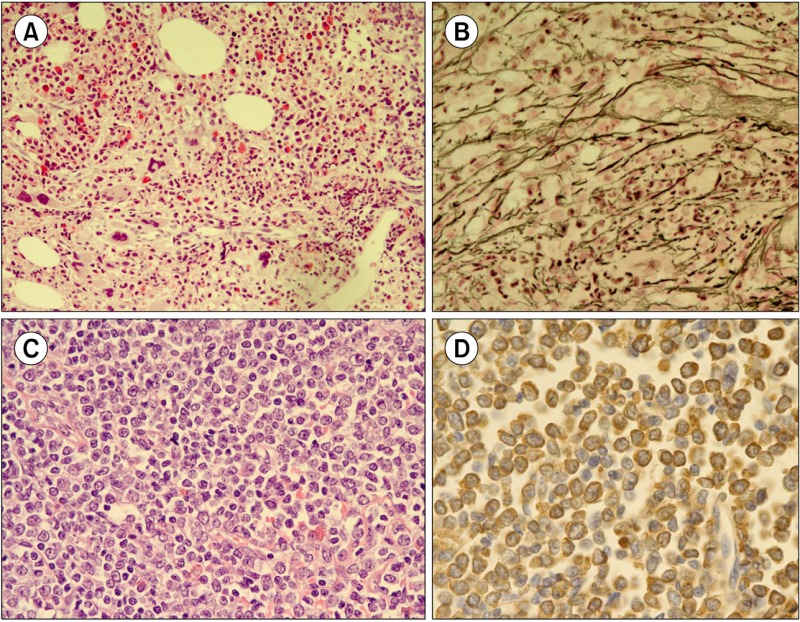
which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. A 54-year-old man was referred to our hospital with right flank pain. Three years ago, he was diagnosed with gastric mucosa-associated lymphoid tissue (MALT) lymphoma and successfully treated with radiotherapy. CBC showed a WBC count of 24. Bone marrow (BM) examination showed granulocytic and megakaryocytic proliferation with moderate dysplastic megakaryopoiesis (A; H&E stain, ×200), and diffuse reticulin fibrosis (B; reticulin stain, ×400). Primary myelofibrosis was the first diagnostic consideration after BM study. Chromosomal analysis, however, showed t(9;22)(q34;q11.2), indicating CML. Concurrent abdomen computerized tomography revealed enlarged inguinal lymph nodes. Inguinal lymph node biopsy showed diffuse infiltration of immature cells (C; H&E stain, ×400), which were positive for myeloperoxidase (D). BCR/ABL1 rearrangement was demonstrated by fluorescence in-situ hybridization analysis, and a diagnosis of granulocytic sarcoma (GS) was made. Accompanying extramedullary myeloid tumor, CML was classified as blastic phase. Secondary CML with a simultaneous manifestation of GS is rare. Combining morphological and molecular-cytogenetic approaches can help detect the coexistence of both neoplasms, especially in CML cases with fewer typical morphologic features.
继发性CML伴骨髓纤维化的髓外细胞危象。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


