Prognostic relevance of pericardial effusion in patients with malignant diseases.
The Korean Journal of Hematology
Pub Date : 2012-09-01
Epub Date: 2012-09-25
DOI:10.5045/kjh.2012.47.3.237
引用次数: 17
Abstract
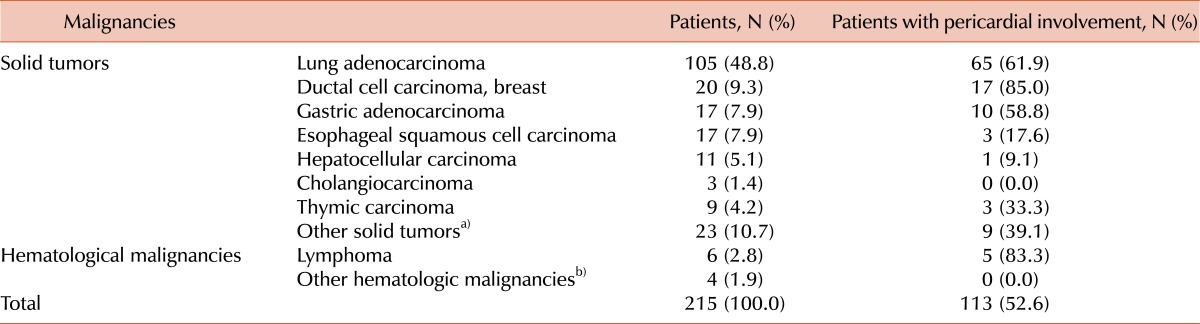
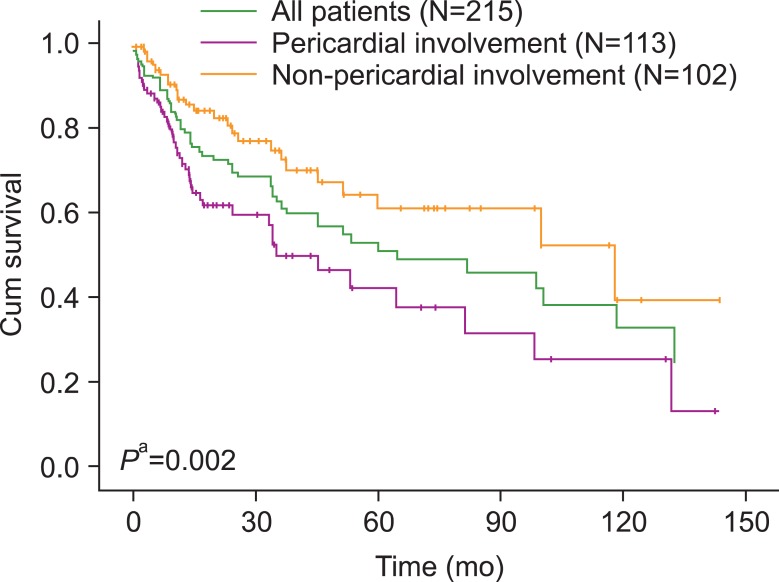
TO THE EDITOR: Malignancy is a common cause of pericardial effusion, and malignant pericardial effusion is a serious manifestation in advanced malignancies [1]. Malignancy-related pericardial effusion is associated with significantly decreased patient survival [1]. Slight malignant pericardial effusions are frequently asymptomatic; however, symptomatic patients often present with cardiac tamponade, which can rapidly lead to cardiovascular collapse or death [2]. Therefore, early diagnosis and timely treatment may decrease a patient's short-term risk of death. We evaluated both the etiology and prognosis of pericardial involvement in several malignancies. We retrospectively reviewed the records of 215 patients (126 males and 89 females) with pericardial effusion and malignant diseases, including solid tumors and hematological malignancies, from January 1991 to December 2010. In all cases, the clinical diagnosis was confirmed by pathological examination of the primary tumor site. All patients underwent pericardiocentesis, and pericardial fluid analyses were performed for cytology. We analyzed the incidence of the etiology of malignancies and overall survival according to the results of the pericardial fluid analysis. Overall survival was calculated from the day of initial diagnosis to the date of patient's death from any other cause or to the latest follow-up date. Among 215 patients, 113 (52.6%) showed pericardial involvement in their malignant diseases. The etiological diagnosis and pericardial fluid analysis results are summarized in Table 1. Pericardial involvement of malignancy was most frequent in breast carcinoma (85.0%), followed by lung adenocarcinoma (61.9%), gastric adenocarcinoma (58.8%), thymic carcinoma (33.3%), and esophageal squamous cell carcinoma (17.6%). In a survival analysis using the Cox proportional hazards model, the pericardial involvement group showed significantly poorer survival rates than the non-pericardial involvement group (hazard ratio, 2.157; 95% confidence interval, 1.327-3.507; P=0.002). The median survival time was significantly longer in patients with no evidence of pericardial involvement in their malignant diseases than in those with pericardial involvement in malignancy (118.2 months vs. 34.8 months; P=0.001) (Fig. 1). Fig. 1 Overall survival according to pericardial involvement in the malignant disease. The pericardial involvement group had a significantly poorer survival rate than the non-pericardial involvement group (Pa, pericardial involvement group vs. non-pericardial ... Table 1 Etiological diagnosis and frequency of pericardial involvement in malignant diseases. In studies, the most common cause of malignant pericardial effusion was lung cancer (34-76%), followed by breast cancer (10-17%) [1, 3, 4]. However, in the present study, ductal cell carcinoma of the breast had the highest incidence of pericardial involvement. Because our study population included only patients with advanced-stage breast cancer, the incidence of their pericardial involvement is not representative of all patients with breast cancer. Several treatment modalities, including both medical and surgical modalities, have been proposed for malignant pericardial effusion [5]. Timely management of pericardial effusion is important to improving the clinical outcome. In conclusion, patients with pericardial involvement in their malignant diseases had a relatively poorer prognosis than those without pericardial involvement in malignant diseases. Cautious morphologic analyses of pericardial fluid are recommended before application of palliative or therapeutic pericardiocentesis, especially in patients with lung or breast carcinoma.
恶性疾病患者心包积液与预后的相关性。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


