C-Jun N-Terminal Kinase 2 Promotes Liver Injury via the Mitochondrial Permeability Transition after Hemorrhage and Resuscitation.
HPB surgery : a world journal of hepatic, pancreatic and biliary surgery
Pub Date : 2012-01-01
Epub Date: 2012-06-27
DOI:10.1155/2012/641982
引用次数: 5
Abstract
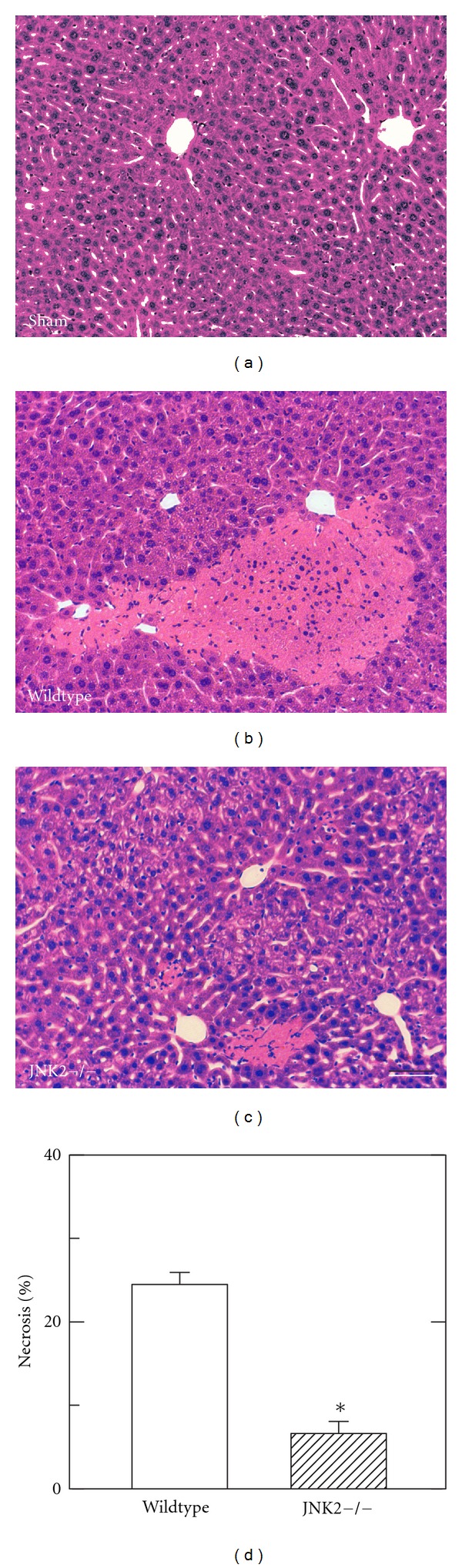
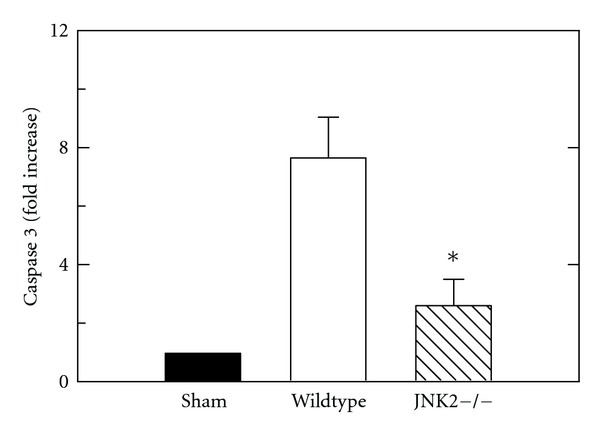
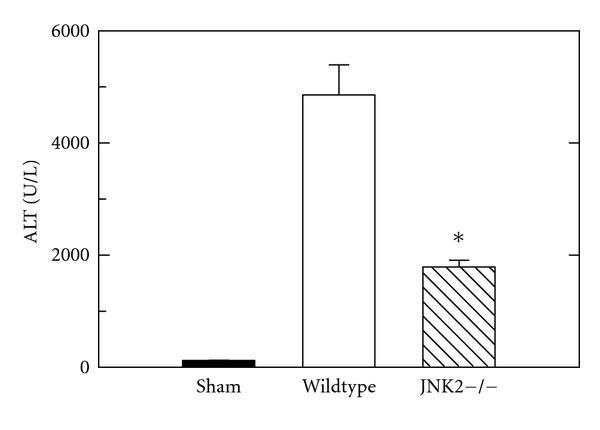
Hemorrhagic shock leads to hepatic hypoperfusion and activation of mitogen-activated stress kinases (MAPK) like c-Jun N-terminal kinase (JNK) 1 and 2. Our aim was to determine whether mitochondrial dysfunction leading to hepatic necrosis and apoptosis after hemorrhage/resuscitation (H/R) was dependent on JNK2. Under pentobarbital anesthesia, wildtype (WT) and JNK2 deficient (KO) mice were hemorrhaged to 30 mm Hg for 3 h and then resuscitated with shed blood plus half the volume of lactated Ringer's solution. Serum alanine aminotransferase (ALT), necrosis, apoptosis and oxidative stress were assessed 6 h after resuscitation. Mitochondrial polarization was assessed by intravital microscopy. After H/R, ALT in WT-mice increased from 130 U/L to 4800 U/L. In KO-mice, ALT after H/R was blunted to 1800 U/l (P < 0.05). Necrosis, caspase-3 activity and ROS were all substantially decreased in KO compared to WT mice after H/R. After sham operation, intravital microscopy revealed punctate mitochondrial staining by rhodamine 123 (Rh123), indicating normal mitochondrial polarization. At 4 h after H/R, Rh123 staining became dim and diffuse in 58% of hepatocytes, indicating depolarization and onset of the mitochondrial permeability transition (MPT). By contrast, KO mice displayed less depolarization after H/R (23%, P < 0.05). In conclusion, JNK2 contributes to MPT-mediated liver injury after H/R.
C-Jun n -末端激酶2通过出血和复苏后线粒体通透性转变促进肝损伤。
失血性休克导致肝灌注不足和丝裂原激活应激激酶(MAPK)如c-Jun n-末端激酶(JNK) 1和2的激活。我们的目的是确定线粒体功能障碍导致出血/复苏后肝坏死和凋亡(H/R)是否依赖于JNK2。在戊巴比妥麻醉下,野生型(WT)和JNK2缺陷型(KO)小鼠出血至30 mm Hg,持续3小时,然后用流出的血加一半体积的乳酸林格氏液复苏。复苏后6 h检测血清丙氨酸转氨酶(ALT)、坏死、细胞凋亡及氧化应激。活体显微镜观察线粒体极化。H/R后,wt -小鼠的ALT由130 U/L增加到4800 U/L。H/R后ko -小鼠ALT降至1800 U/l (P < 0.05)。与WT小鼠相比,H/R后KO小鼠的坏死、caspase-3活性和ROS均显著降低。假手术后,活体显微镜显示罗丹明123 (Rh123)点状线粒体染色,表明线粒体极化正常。h /R后4 h, 58%的肝细胞Rh123染色变暗且弥散,表明去极化和线粒体通透性转变(MPT)开始。相比之下,KO小鼠经H/R后去极化程度降低(23%,P < 0.05)。总之,JNK2参与了H/R后mpt介导的肝损伤。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


