Effects of dietary salt restriction on puromycin aminonucleoside nephrosis: preliminary data.
Q3 Medicine
Electrolyte and Blood Pressure
Pub Date : 2011-12-01
Epub Date: 2011-12-31
DOI:10.5049/EBP.2011.9.2.55
引用次数: 2
Abstract
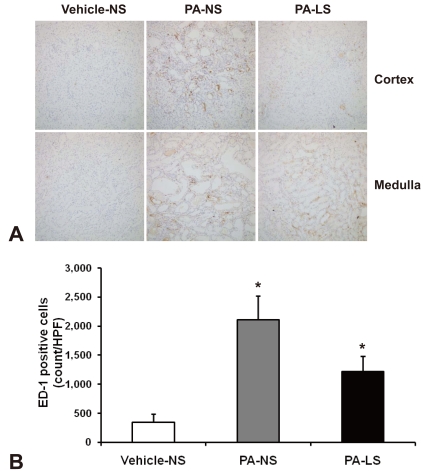
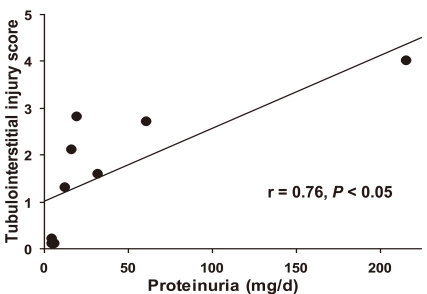
Proteinuria is a major promoter that induces tubulointerstitial injury in glomerulopathy. Dietary salt restriction may reduce proteinuria, although the mechanism is not clear. We investigated the effects of dietary salt restriction on rat kidneys in an animal model of glomerular proteinuria. Male Sprague-Dawley rats were used and divided into 3 groups: vehicle-treated normal-salt controls, puromycin aminonucleoside (PA)-treated normal-salt rats, and PA-treated low-salt rats. PA was given at a dose of 150 mg/kg BW at time 0, followed by 50 mg/kg BW on days 28, 35, and 42. Sodium-deficient rodent diet with and without additional NaCl (0.5%) were provided for normal-salt rats and low-salt rats, respectively. On day 63, kidneys were harvested for histopathologic examination and immunohistochemistry. PA treatment produced overt proteinuria and renal damage. Dietary salt restriction insignificantly reduced proteinuria in PA-treated rats, and PA-treated low-salt rats had lower urine output and lower creatinine clearance than vehicle-treated normal-salt controls. When tubulointerstitial injury was semiquantitatively evaluated, it had a positive correlation with proteinuria. The tubulointerstitial injury score was significantly increased by PA treatment and relieved by low-salt diet. ED1-positive infiltrating cells and immunostaining for interstitial collagen III were significantly increased by PA treatment. These changes appeared to be less common in PA-treated low-salt rats, although the differences in PA-treated normal-salt versus low-salt rats did not reach statistical significance. Our results suggest that renal histopathology in PA nephrosis may potentially be improved by dietary salt restriction. Non-hemodynamic mechanisms induced by low-sodium diet might contribute to renoprotection.

饮食盐限制对嘌呤霉素氨基核苷肾病的影响:初步数据。
蛋白尿是肾小球病变中诱导小管间质损伤的主要启动子。饮食盐限制可能减少蛋白尿,尽管机制尚不清楚。我们在肾小球蛋白尿动物模型中研究了饮食盐限制对大鼠肾脏的影响。选取雄性Sprague-Dawley大鼠,分为3组:正常盐对照、嘌呤霉素氨基核苷(PA)处理正常盐大鼠和PA处理低盐大鼠。在第0天给予150 mg/kg BW的PA,随后在第28、35和42天给予50 mg/kg BW。正常盐大鼠和低盐大鼠分别饲喂加0.5% NaCl和不加0.5% NaCl的缺钠鼠粮。第63天,取肾进行组织病理学检查和免疫组织化学。PA治疗产生明显的蛋白尿和肾脏损害。饮食盐限制没有显著减少pa处理大鼠的蛋白尿,并且pa处理的低盐大鼠的尿量和肌酐清除率低于正常盐处理的对照组。当半定量评估小管间质损伤时,它与蛋白尿呈正相关。PA治疗后小管间质损伤评分显著升高,低盐饮食减轻。PA处理后,ed1阳性浸润细胞和间质III型胶原免疫染色明显增加。这些变化在pa处理的低盐大鼠中似乎不太常见,尽管pa处理的正常盐与低盐大鼠的差异没有达到统计学意义。我们的研究结果表明,PA肾病的肾脏组织病理学可能通过限制饮食盐而得到改善。低钠饮食诱导的非血流动力学机制可能有助于肾保护。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


