Multiparametric breast MRI to problem-solve mammographically detected suspicious calcifications
IF 3.3
3区 医学
Q1 RADIOLOGY, NUCLEAR MEDICINE & MEDICAL IMAGING
引用次数: 0
Abstract
Objective
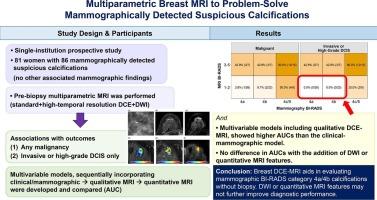
To evaluate the performance of multiparametric breast MRI to problem-solve mammographically-detected suspicious calcifications.
Materials and methods
Participants with mammographically-detected suspicious calcifications were prospectively enrolled between August 2017 to May 2023. Pre-biopsy multiparametric MRI (standard and high-temporal resolution dynamic contrast enhanced [DCE]-MRI acquisitions and diffusion-weighted imaging [DWI]) was performed. The associations of MRI features with outcomes – (1) any malignancy and (2) invasive or high-grade ductal carcinoma in situ [DCIS] only – were analyzed using univariable logistic regression. Multivariable models, sequentially incorporating clinical/mammographic, qualitative, and quantitative features, were developed using penalized logistic regression with the least absolute shrinkage and selection operator. Area under the receiver operating characteristic curves (AUC) were estimated via cross-validation and compared between models using bootstrap methods.
Results
81 women (mean age, 55 years ± 10 [standard deviation]) with 86 calcifications were included; 29 % (25/86) were malignant. Malignancy rates for non-enhancing mammographic Breast Imaging Reporting and Data System (BI-RADS) category 4a and 4b calcifications were 3.8 % (1/26) and 8.7 % (2/23), respectively, with no invasive cancer or high-grade DCIS. Mammographic BI-RADS category, MRI BI-RADS category, visibility on DWI, peak percent enhancement, functional tumor volume, and Ktrans values were associated with both outcomes (all p < 0.05). Multivariable models, including qualitative DCE-MRI assessments, showed higher AUCs (malignancy: 0.71–0.76; invasive cancer or high-grade DCIS: 0.78–0.91) than when including only clinical and mammographic features (malignancy: 0.57; invasive cancer or high-grade DCIS: 0.61, all p < 0.05). Further incorporation of DWI or quantitative MRI features did not improve AUCs (all ΔAUC ≤ 0).
Conclusion
Breast DCE-MRI aids in evaluating mammographic BI-RADS category 4a/4b calcifications without biopsy. DWI or quantitative MRI features may not further improve diagnostic performance.
多参数乳房MRI解决乳房x光检查发现可疑钙化的问题。
目的:评价多参数乳腺MRI在解决乳房x线检查可疑钙化问题中的应用价值。材料和方法:在2017年8月至2023年5月期间前瞻性纳入乳房x线检查检测到可疑钙化的参与者。活检前进行多参数MRI(标准和高时间分辨率动态对比增强[DCE]-MRI采集和扩散加权成像[DWI])。MRI特征与预后(1)任何恶性肿瘤和(2)侵袭性或高级别导管原位癌[DCIS])的关联使用单变量logistic回归分析。多变量模型,依次纳入临床/乳房x线摄影,定性和定量特征,使用惩罚逻辑回归与最小的绝对收缩和选择算子开发。通过交叉验证估计了受试者工作特征曲线下的面积(AUC),并使用bootstrap方法比较了模型之间的差异。结果:纳入81例女性(平均年龄55岁±10岁[标准差]),86例钙化;29%(25/86)为恶性。乳腺成像报告和数据系统(BI-RADS)非增强x线摄影4a和4b类钙化的恶性率分别为3.8%(1/26)和8.7%(2/23),无浸润性癌或高级别DCIS。乳腺造影BI-RADS分类、MRI BI-RADS分类、DWI可见性、峰值增强百分比、功能性肿瘤体积和Ktrans值与两种结果相关(均p)。结论:乳腺DCE-MRI有助于评估乳腺造影BI-RADS 4a/4b类钙化,无需活检。DWI或定量MRI特征可能不能进一步提高诊断性能。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
CiteScore
6.70
自引率
3.00%
发文量
398
审稿时长
42 days
期刊介绍:
European Journal of Radiology is an international journal which aims to communicate to its readers, state-of-the-art information on imaging developments in the form of high quality original research articles and timely reviews on current developments in the field.
Its audience includes clinicians at all levels of training including radiology trainees, newly qualified imaging specialists and the experienced radiologist. Its aim is to inform efficient, appropriate and evidence-based imaging practice to the benefit of patients worldwide.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


