Impact of body mass index on 90-day survival in patients in cardiogenic shock treated with V-A ECMO: A propensity weighted analysis
IF 2.9
3区 医学
Q2 CRITICAL CARE MEDICINE
引用次数: 0
Abstract
Objective
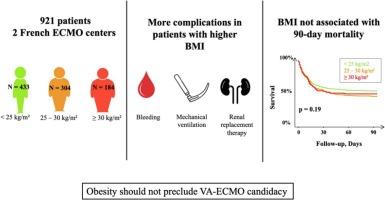
The impact of body mass index (BMI) on outcomes in refractory cardiogenic shock requiring extracorporeal membrane oxygenation (ECMO) is not well understood. We aimed to assess: (i) whether BMI is independently associated with outcomes, and (ii) whether patients with obesity (BMI > 30 kg/m2) have worse outcomes than lean counterparts.
Methods
We conducted a retrospective analysis of a prospectively maintained database from two French ECMO centers (2006–2022). The impact of BMI was evaluated using inverse propensity-score weighted (IPSW), propensity-score (PS) matching, and multivariable (MV) models, adjusting for predefined confounders. The primary outcome was 90-day mortality. The relationship between BMI and outcomes was examined using generalized additive models. Outcomes were compared across three BMI categories (<25 kg/m2, 25-30 kg/m2, and > 30 kg/m2). Patients treated with extracorporeal cardiopulmonary resuscitation (E-CPR) were analyzed separately.
Results
Among 921 patients, BMI was not significantly associated with 90-day mortality (HR 0.99, 95 % CI 0.97–1.01, p = 0.2), despite more ECMO-related complications. This was consistent across PS-matched, IPSW, and MV models. No significant non-linear relationship between BMI and 90-day mortality was found. Among the 204 patients with ECMO during cardiopulmonary resuscitation, those with BMI < or ≥ 30 kg/m2 had 90-day mortality rates of 76 % and 71 %, respectively (p = 0.5).
Conclusion
Patients with obesity treated with ECMO for refractory cardiogenic shock have similar 90-day outcomes to their lean counterparts, despite higher respiratory, renal, and device-related complications.
体重指数对V-A ECMO治疗心源性休克患者90天生存率的影响:倾向加权分析
目的体重指数(BMI)对需要体外膜氧合(ECMO)治疗的难治性心源性休克预后的影响尚不清楚。我们的目的是评估:(i) BMI是否与预后独立相关,以及(ii)肥胖患者(BMI > 30 kg/m2)的预后是否比瘦患者差。方法:我们对两个法国ECMO中心(2006-2022)前瞻性维护的数据库进行回顾性分析。BMI的影响采用反向倾向评分加权(IPSW)、倾向评分匹配(PS)和多变量(MV)模型进行评估,并对预定义混杂因素进行调整。主要终点为90天死亡率。使用广义加性模型检验BMI与预后之间的关系。比较了三个BMI类别(25 kg/m2、25-30 kg/m2和30 kg/m2)的结果。采用体外心肺复苏(E-CPR)治疗的患者分别进行分析。结果在921例患者中,尽管有更多的ecmo相关并发症,但BMI与90天死亡率无显著相关性(HR 0.99, 95% CI 0.97-1.01, p = 0.2)。这在ps匹配、IPSW和MV模型中是一致的。BMI与90天死亡率之间没有明显的非线性关系。204例心肺复苏期间ECMO患者中,BMI≥30 kg/m2的患者90天死亡率分别为76%和71% (p = 0.5)。结论:采用ECMO治疗难治性心源性休克的肥胖患者90天的预后与消瘦患者相似,尽管呼吸、肾脏和器械相关并发症更高。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Journal of critical care
医学-危重病医学
CiteScore
8.60
自引率
2.70%
发文量
237
审稿时长
23 days
期刊介绍:
The Journal of Critical Care, the official publication of the World Federation of Societies of Intensive and Critical Care Medicine (WFSICCM), is a leading international, peer-reviewed journal providing original research, review articles, tutorials, and invited articles for physicians and allied health professionals involved in treating the critically ill. The Journal aims to improve patient care by furthering understanding of health systems research and its integration into clinical practice.
The Journal will include articles which discuss:
All aspects of health services research in critical care
System based practice in anesthesiology, perioperative and critical care medicine
The interface between anesthesiology, critical care medicine and pain
Integrating intraoperative management in preparation for postoperative critical care management and recovery
Optimizing patient management, i.e., exploring the interface between evidence-based principles or clinical insight into management and care of complex patients
The team approach in the OR and ICU
System-based research
Medical ethics
Technology in medicine
Seminars discussing current, state of the art, and sometimes controversial topics in anesthesiology, critical care medicine, and professional education
Residency Education.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


