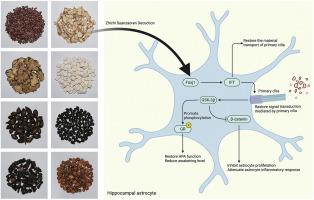
Zhichi Suanzaoren Decoction alleviates perimenopausal insomnia via restoring astrocytic primary cilia and modulating Wnt/GSK-3β/GR signaling axis
IF 5.4
2区 医学
Q1 CHEMISTRY, MEDICINAL
引用次数: 0
Abstract
Ethnopharmacological relevance
Traditional Chinese medicine has historically used Zhichi Suanzaoren Decoction (ZSD) to alleviate perimenopausal insomnia (PMI). ZSD has demonstrated clinical efficacy in treating PMI-related symptoms; however, its active constituents and mechanisms of action remain unclear.
Aim of the study
The aim of this study was to explore the bioactive components of ZSD using UPLC-Q-TOF/MS, evaluate its efficacy in vivo experiments, and elucidate its potential mechanisms of action—particularly the role of primary hippocampal astrocyte cilia in PMI.
Materials and methods
The main components of ZSD were analyzed by UPLC-Q-TOF/MS. A PMI model was established using bilateral ovariectomy, followed by ZSD treatment. Behavioral tests and pentobarbital sodium-induced sleep synergy experiments were used to assess anti-insomnia and anxiolytic effects. Mechanistic studies included ELISA, Nissl staining, immunohistochemistry, transcriptome sequencing, immunofluorescence staining, qRT-PCR, Western blotting, and adeno-associated virus (AAV)-mediated Foxj1 knockdown.
Results
A total of 97 chemical components in the aqueous extract of ZSD were identified using UPLC-Q-TOF/MS in positive- and negative-ion modes. ZSD significantly improved sleep and reduced anxiety in PMI mice; increased hippocampal GABA levels; and reduced serum ACTH, CORT, IL-6, TNF-α, and IL-1β levels. ZSD exerts a protective effect on hippocampal neurons and reduces neuroinflammation. Transcriptomic and protein-level analyses demonstrated that ZSD inhibited Wnt signaling by promoting Foxj1 expression and restoring primary cilia in astrocytes. This led to dual effects: (1) activation of the GSK-3β/GR signaling pathway, restoring HPA axis function and reversing glucocorticoid resistance; and (2) suppression of β-catenin nuclear translocation and astrocyte-driven neuroinflammation.
Conclusions
ZSD can alleviate insomnia, anxiety, and neuroinflammation in a PMI model. The therapeutic effects are mediated through the restoration of primary astrocyte cilia via Foxj1 upregulation. These findings highlight a previously unrecognized role of primary cilia in the pathogenesis of PMI and provide a scientific rationale for the clinical application of ZSD and traditional Chinese medicine in mood-related disorders.
止泻酸早人汤通过修复星形细胞原发纤毛、调节Wnt/GSK-3β/GR信号轴改善围绝经期失眠。
民族药理学相关性:中药历史上使用止泻酸枣人汤(ZSD)缓解围绝经期失眠(PMI)。ZSD在治疗pmi相关症状方面具有临床疗效;然而,其有效成分和作用机制尚不清楚。研究目的:本研究的目的是利用UPLC-Q-TOF/MS技术探索ZSD的生物活性成分,评估其体内实验的疗效,并阐明其潜在的作用机制,特别是海马原代星形细胞纤毛在PMI中的作用。材料与方法:采用UPLC-Q-TOF/MS对ZSD的主要成分进行分析。采用双侧卵巢切除术和ZSD治疗建立PMI模型。采用行为测试和戊巴比妥钠诱导睡眠协同实验评估其抗失眠和抗焦虑作用。机制研究包括ELISA、尼氏染色、免疫组织化学、转录组测序、免疫荧光染色、qRT-PCR、Western blotting和腺相关病毒(AAV)介导的Foxj1敲低。结果:采用UPLC-Q-TOF/MS,在正离子和负离子模式下鉴定出了ZSD水提液中的97种化学成分。ZSD显著改善PMI小鼠睡眠,减少焦虑;海马GABA水平升高;降低血清ACTH、CORT、IL-6、TNF-α和IL-1β水平。ZSD对海马神经元有保护作用,减轻神经炎症。转录组学和蛋白水平分析表明,ZSD通过促进Foxj1表达和恢复星形胶质细胞的初级纤毛来抑制Wnt信号传导。这导致了双重作用:(1)激活GSK-3β/GR信号通路,恢复HPA轴功能,逆转糖皮质激素抵抗;(2) β-catenin核易位和星形胶质细胞驱动的神经炎症的抑制。结论:在PMI模型中,ZSD可以减轻失眠、焦虑和神经炎症。其治疗效果是通过Foxj1上调介导星形胶质细胞原代纤毛的修复。这些发现突出了以前未被认识到的初级纤毛在PMI发病机制中的作用,并为ZSD和中医在情绪相关疾病中的临床应用提供了科学依据。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Journal of ethnopharmacology
医学-全科医学与补充医学
CiteScore
10.30
自引率
5.60%
发文量
967
审稿时长
77 days
期刊介绍:
The Journal of Ethnopharmacology is dedicated to the exchange of information and understandings about people''s use of plants, fungi, animals, microorganisms and minerals and their biological and pharmacological effects based on the principles established through international conventions. Early people confronted with illness and disease, discovered a wealth of useful therapeutic agents in the plant and animal kingdoms. The empirical knowledge of these medicinal substances and their toxic potential was passed on by oral tradition and sometimes recorded in herbals and other texts on materia medica. Many valuable drugs of today (e.g., atropine, ephedrine, tubocurarine, digoxin, reserpine) came into use through the study of indigenous remedies. Chemists continue to use plant-derived drugs (e.g., morphine, taxol, physostigmine, quinidine, emetine) as prototypes in their attempts to develop more effective and less toxic medicinals.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


