Well-differentiated grade 1 and 2 nonfunctioning pancreatic neuroendocrine tumor: Consideration of additional factors to aid treatment decision-making
IF 2.7
3区 医学
Q1 SURGERY
引用次数: 0
Abstract
Background
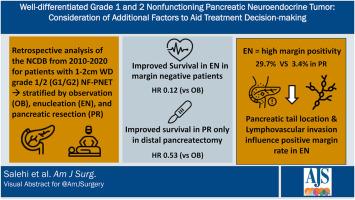
Guidelines for 1–2 cm well-differentiated non-functional pancreatic neuroendocrine tumors (NF-PNET) are broad; observation (OB), enucleation (EN), and pancreatic resection (PR) all viable. The objective is analyzing factors impacting survival between approaches.
Methods
Retrospective analysis of NCDB for 1–2 cm well-differentiated grade 1/2 NF-PNET stratified by approach. Factors predicting survival analyzed using Cox regression.
Results
4023 patients included; 1030 OB, 321 EN, and 2672 PR. EN was associated with improved survival (HR 0.20, 95 %CI 0.08–0.53) and was dependent on negative margins (margin negative: HR 0.12, 95 %CI 0.05–0.34). Positive margins for EN were high (29.7 % EN vs. 3.4 % PR, p < 0.01). Factors influencing margins for EN were pancreatic tail location (OR 0.36, 95 %CI 0.13–0.98) and lymphovascular invasion (OR 5.28, 95 %CI 1.42–19.53). Among PRs, only distal pancreatectomy conferred improved survival (HR 0.53, 95 %CI 0.30–0.92).
Conclusion
Optimal treatment for 1–2 cm well-differentiated NF-PNET should incorporate factors influencing positive margins for EN and resection type for PR.
高分化1级和2级无功能胰腺神经内分泌肿瘤:考虑辅助治疗决策的其他因素
背景:1-2厘米高分化非功能性胰腺神经内分泌肿瘤(NF-PNET)的指南是广泛的;观察(OB),去核(EN)和胰腺切除术(PR)均可行。目的是分析不同方法之间影响生存率的因素。方法回顾性分析1 ~ 2 cm高分化1/2 NF-PNET患者的NCDB。使用Cox回归分析预测生存的因素。结果纳入4023例患者;1030 OB, 321 EN和2672 PR。EN与改善的生存率相关(HR 0.20, 95% CI 0.08-0.53),并依赖于阴性切缘(切缘阴性:HR 0.12, 95% CI 0.05-0.34)。EN的阳性利润率很高(29.7% EN vs. 3.4% PR, p < 0.01)。影响EN边缘的因素是胰腺尾部位置(OR = 0.36, 95% CI = 0.13-0.98)和淋巴血管浸润(OR = 5.28, 95% CI = 1.42-19.53)。在pr中,只有远端胰腺切除术提高了生存率(HR 0.53, 95% CI 0.30-0.92)。结论1 ~ 2cm高分化NF-PNET的最佳治疗应综合考虑EN阳性切缘的影响因素和PR切除类型的影响因素。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
CiteScore
5.00
自引率
6.70%
发文量
570
审稿时长
56 days
期刊介绍:
The American Journal of Surgery® is a peer-reviewed journal designed for the general surgeon who performs abdominal, cancer, vascular, head and neck, breast, colorectal, and other forms of surgery. AJS is the official journal of 7 major surgical societies* and publishes their official papers as well as independently submitted clinical studies, editorials, reviews, brief reports, correspondence and book reviews.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


