Application of nutrition interventions with GLP-1 based therapies: A narrative review of the challenges and solutions
引用次数: 0
Abstract
Background
Obesity is a heterogeneous systemic chronic disease associated with excess adiposity and a complex etiology and is increasing in prevalence worldwide. Initially used to treat type 2 diabetes mellitus, glucagon-like peptide-1 (GLP-1) based therapies are now widely prescribed for individuals with overweight and obesity as an adjunct to a reduced-calorie diet and increased physical activity. However, despite their impressive weight reduction capabilities, many patients on GLP-1 based therapies do not receive appropriate nutrition advice and struggle to maintain their weight reduction.
Methods
This narrative review explores and summarizes existing literature on the challenges associated with nutrition intake in people with obesity taking GLP-1 based therapies and practical applications of nutrition and lifestyle interventions for the management of these individuals to ensure their best long-term health outcomes.
Results
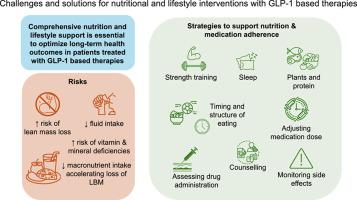
Delivering optimal nutrition management to people with obesity treated with GLP-1 based therapies presents healthcare providers with many challenges including addressing the impact of obesity and weight reduction on body composition (particularly muscle mass loss and risk of sarcopenic obesity), and poor nutrition. Physicians should work with dietitians and other healthcare providers to deliver comprehensive lifestyle counselling that is patient-centered, aligning with the needs and preferences of the individual. This should include advice on: timely and appropriate nutrition that centers on adequate macronutrient, micronutrient and fluid intake, particularly increased protein intake alongside resistance training for the preservation of muscle mass; mental health; sleep hygiene, physical activity; and medication adherence and persistence. Evidence-based nutrition guidelines can also provide an important framework for healthcare professionals, helping to ensure nutrition advice is consistent and based on rigorous scientific research.
Conclusions
Our findings underscore the importance of ensuring that patients treated with GLP-1 based therapies are closely monitored and provided with comprehensive nutrition and lifestyle support to ensure they achieve the best long-term health outcomes.
基于GLP-1疗法的营养干预的应用:挑战和解决方案的叙述性回顾
背景:肥胖是一种与过度肥胖相关的异质性全身性慢性疾病,病因复杂,在世界范围内的患病率正在上升。最初用于治疗2型糖尿病,以胰高血糖素样肽-1 (GLP-1)为基础的疗法现在广泛用于超重和肥胖患者,作为减少卡路里饮食和增加体育锻炼的辅助手段。然而,尽管GLP-1具有令人印象深刻的减肥能力,但许多接受GLP-1为基础的治疗的患者没有得到适当的营养建议,并且很难保持他们的减肥效果。方法本综述对现有文献进行了探讨和总结,探讨了肥胖患者采用基于GLP-1的治疗方法与营养摄入相关的挑战,以及对这些个体进行营养和生活方式干预的实际应用,以确保其最佳的长期健康结果。结果:为接受GLP-1治疗的肥胖患者提供最佳营养管理给医疗保健提供者带来了许多挑战,包括解决肥胖和体重减轻对身体成分的影响(特别是肌肉质量减少和肌肉减少性肥胖的风险),以及营养不良。医生应该与营养师和其他医疗保健提供者合作,提供以患者为中心的全面生活方式咨询,与个人的需求和偏好保持一致。这应包括以下方面的建议:及时和适当的营养,以充足的宏量营养素、微量营养素和液体摄入为中心,特别是增加蛋白质摄入量,同时进行阻力训练以保持肌肉质量;心理健康;睡眠卫生,身体活动;药物依从性和持久性。以证据为基础的营养指南还可以为卫生保健专业人员提供一个重要的框架,帮助确保营养建议的一致性,并以严格的科学研究为基础。结论:我们的研究结果强调了确保接受GLP-1治疗的患者受到密切监测并提供全面的营养和生活方式支持的重要性,以确保他们获得最佳的长期健康结果。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


