Development and validation of machine learning predictive models for gastric volume based on ultrasonography: A multicentre study
IF 5.1
2区 医学
Q1 ANESTHESIOLOGY
引用次数: 0
Abstract
Study objective
Aspiration of gastric contents is a serious complication associated with anaesthesia. Accurate prediction of gastric volume may assist in risk stratification and help prevent aspiration. This study aimed to develop and validate machine learning models to predict gastric volume based on ultrasound and clinical features.
Methods
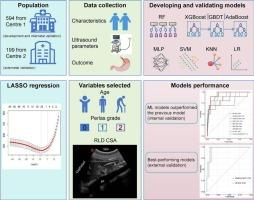
This cross-sectional multicentre study was conducted at two hospitals and included adult patients undergoing gastroscopy under intravenous anaesthesia. Patients from Centre 1 were prospectively enrolled and randomly divided into a training set (Cohort A, n = 415) and an internal validation set (Cohort B, n = 179), while patients from Centre 2 were used as an external validation set (Cohort C, n = 199). The primary outcome was gastric volume, which was measured by endoscopic aspiration immediately following ultrasonographic examination. Least absolute shrinkage and selection operator (LASSO) regression was used for feature selection, and eight machine learning models were developed and evaluated using Bland-Altman analysis. The models' ability to predict medium-to-high and high gastric volumes was assessed. The top-performing models were externally validated, and their predictive performance was compared with the traditional Perlas model.
Main results
Among the 793 enrolled patients, the number and proportion of patients with high gastric volume were as follows: 23 (5.5 %) in the development cohort, 10 (5.6 %) in the internal validation cohort, and 3 (1.5 %) in the external validation cohort. Eight models were developed using age, cross-sectional area of gastric antrum in right lateral decubitus (RLD-CSA) position, and Perlas grade, with these variables selected through LASSO regression. In internal validation, Bland-Altman analysis showed that the Perlas model overestimated gastric volume (mean bias 23.5 mL), while the new models provided accurate estimates (mean bias −0.1 to 2.0 mL). The models significantly improved prediction of medium-high gastric volume (area under the curve [AUC]: 0.74–0.77 vs. 0.63) and high gastric volume (AUC: 0.85–0.94 vs. 0.74). The best-performing adaptive boosting and linear regression models underwent externally validation, with AUCs of 0.81 (95 % confidence interval [CI], 0.74–0.89) and 0.80 (95 %CI, 0.72–0.89) for medium-high and 0.96 (95 %CI, 0.91–1) and 0.96 (95 %CI, 0.89–1) for high gastric volume.
Conclusions
We propose a novel machine learning-based predictive model that outperforms Perlas model by incorporating the key features of age, RLD-CSA, and Perlas grade, enabling accurate prediction of gastric volume.
基于超声的胃容积机器学习预测模型的开发和验证:一项多中心研究。
研究目的:胃内容物误吸是与麻醉相关的严重并发症。准确预测胃容量可能有助于风险分层,并有助于防止误吸。本研究旨在开发和验证基于超声和临床特征预测胃体积的机器学习模型。方法:本横断面多中心研究在两家医院进行,包括在静脉麻醉下进行胃镜检查的成年患者。来自中心1的患者被前瞻性纳入,随机分为训练集(队列a, n = 415)和内部验证集(队列B, n = 179),而来自中心2的患者被用作外部验证集(队列C, n = 199)。主要结果是胃容量,在超声检查后立即通过内窥镜抽吸测量胃容量。最小绝对收缩和选择算子(LASSO)回归用于特征选择,并开发了8个机器学习模型,并使用Bland-Altman分析进行了评估。评估了模型预测中、高和高胃容量的能力。对表现最好的模型进行了外部验证,并将其预测性能与传统的Perlas模型进行了比较。主要结果:793例入组患者中,高胃容量患者的数量和比例如下:开发组23例(5.5%),内部验证组10例(5.6%),外部验证组3例(1.5%)。采用年龄、右侧卧位胃窦横截面积(RLD-CSA)和Perlas分级建立8个模型,并通过LASSO回归选择这些变量。在内部验证中,Bland-Altman分析显示Perlas模型高估了胃容量(平均偏差23.5 mL),而新模型提供了准确的估计(平均偏差-0.1至2.0 mL)。该模型显著改善了对中高胃容量(曲线下面积[AUC]: 0.74-0.77 vs. 0.63)和高胃容量(AUC: 0.85-0.94 vs. 0.74)的预测。表现最佳的自适应增强和线性回归模型进行了外部验证,中高胃容量的auc为0.81(95%可信区间[CI], 0.74-0.89)和0.80 (95% CI, 0.72-0.89),高胃容量的auc为0.96 (95% CI, 0.91-1)和0.96 (95% CI, 0.89-1)。结论:我们提出了一种新的基于机器学习的预测模型,通过结合年龄、RLD-CSA和Perlas分级的关键特征,该模型优于Perlas模型,能够准确预测胃容量。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
CiteScore
7.40
自引率
4.50%
发文量
346
审稿时长
23 days
期刊介绍:
The Journal of Clinical Anesthesia (JCA) addresses all aspects of anesthesia practice, including anesthetic administration, pharmacokinetics, preoperative and postoperative considerations, coexisting disease and other complicating factors, cost issues, and similar concerns anesthesiologists contend with daily. Exceptionally high standards of presentation and accuracy are maintained.
The core of the journal is original contributions on subjects relevant to clinical practice, and rigorously peer-reviewed. Highly respected international experts have joined together to form the Editorial Board, sharing their years of experience and clinical expertise. Specialized section editors cover the various subspecialties within the field. To keep your practical clinical skills current, the journal bridges the gap between the laboratory and the clinical practice of anesthesiology and critical care to clarify how new insights can improve daily practice.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


