Development of a Unified Geriatric Emergency Department Database, 2022.
IF 5
1区 医学
Q1 EMERGENCY MEDICINE
引用次数: 0
Abstract
STUDY OBJECTIVE Recent initiatives have aimed to improve emergency care for older adults by supporting the recognition of geriatric emergency departments (GEDs). Our objective was to create a unified database of GEDs to understand the distribution and growth of US GEDs. METHODS We identified United States emergency departments (EDs) that were members of the Geriatric ED Collaborative (GEDC) or accredited by the Geriatric ED Accreditation (GEDA) program by December 31, 2022. For completeness, we also identified hospitals recognized by the Age Friendly Health Systems (AFHS), although this recognition is not ED-specific. We collected the year each facility first received recognition and incorporated the combined list into the 2022 National ED Inventory-US database. RESULTS We identified 324 GEDs (5.8%) among 5,622 nonfederal EDs in 2022. An additional 202 hospitals were recognized by AFHS, yielding 526 (9.4%) potential GEDs (pGEDs). GEDs (and pGEDs) were disproportionally located in urban areas. From 2017 to 2019, 110 (69%) of 160 pGEDs were in nonteaching hospitals, and from 2020 to 2022, 316 (86%) of 366 were. This rise in nonteaching hospital pGEDs was driven largely by AFHS hospitals, but a similar pattern was observed among GEDs (GEDC and GEDA). Attainment of GEDA was more likely among EDs in GEDC (odds ratio 13.56, 95% confidence interval 6.14 to 29.96) than AFHS-recognized hospitals (odds ratio 3.26, 95% confidence interval 2.15 to 4.95). CONCLUSIONS The different requirements of GEDC, GEDA, and AFHS-along with current findings-support inclusion of GEDC or GEDA only in the unified national GED database. Furthermore, there was an increase in the number of pGEDs in nonteaching hospitals since 2017. We encourage further efforts to expand these 2 ED-based programs into nonurban, community EDs.发展统一的老年急诊科数据库,2022年。
研究目的最近的举措旨在通过支持对老年急诊科(GEDs)的认可来改善老年人的急诊护理。我们的目标是创建一个统一的普通高等教育数据库,以了解美国普通高等教育的分布和增长情况。方法我们在2022年12月31日之前确定了美国急诊科(ED),这些急诊科(ED)是老年ED协作(GEDC)的成员或获得老年ED认证(GEDA)计划的认证。为了完整起见,我们还确定了由老年友好卫生系统(AFHS)认可的医院,尽管这种认可不是针对ed的。我们收集了每个设施首次获得认可的年份,并将合并列表纳入2022年国家ED库存-美国数据库。结果我们在2022年的5,622名非联邦ed中鉴定出324名ged(5.8%)。另有202家医院获得了AFHS的认可,产生了526家(9.4%)潜在的ged (pged)。普通高等教育(和普通高等教育)不成比例地分布在城市地区。2017年至2019年,160名pged中有110名(69%)在非教学医院,2020年至2022年,366名pged中有316名(86%)在非教学医院。非教学医院pged的增加主要是由AFHS医院推动的,但在普通教育医院(GEDC和GEDA)中也观察到类似的模式。GEDC的急诊达到GEDA的可能性高于afhs认可的医院(优势比为13.56,95%可信区间为6.14 ~ 29.96)(优势比为3.26,95%可信区间为2.15 ~ 4.95)。结论GEDC、GEDA和afhs的不同要求以及目前的研究结果支持将GEDC或GEDA仅纳入国家统一的GED数据库。此外,自2017年以来,非教学医院的pged人数有所增加。我们鼓励进一步努力将这两个基于教育的项目扩展到非城市的社区教育。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
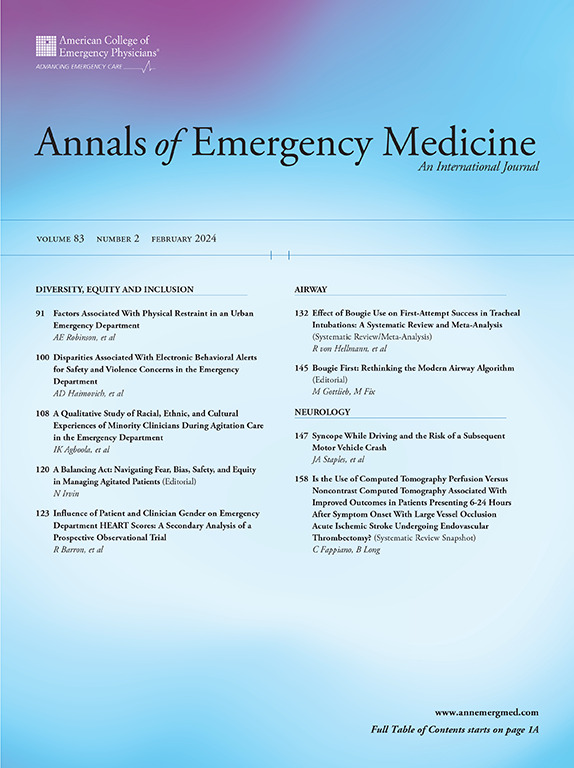
Annals of emergency medicine
医学-急救医学
CiteScore
8.30
自引率
4.80%
发文量
819
审稿时长
20 days
期刊介绍:
Annals of Emergency Medicine, the official journal of the American College of Emergency Physicians, is an international, peer-reviewed journal dedicated to improving the quality of care by publishing the highest quality science for emergency medicine and related medical specialties. Annals publishes original research, clinical reports, opinion, and educational information related to the practice, teaching, and research of emergency medicine. In addition to general emergency medicine topics, Annals regularly publishes articles on out-of-hospital emergency medical services, pediatric emergency medicine, injury and disease prevention, health policy and ethics, disaster management, toxicology, and related topics.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


