Chronic kidney disease- mineral and bone disorder in autosomal dominant policystic kidney disease
IF 3.6
2区 医学
Q2 ENDOCRINOLOGY & METABOLISM
引用次数: 0
Abstract
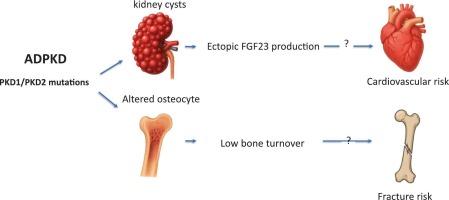
Autosomal dominant polycystic kidney disease (ADPKD) is the most common genetic disorder characterized by bilateral renal cysts that detach from parental tubules, progressively leading to renal function loss. Patients with ADPKD represent a unique subset of chronic kidney disease (CKD) individuals, sharing common CKD features while also exhibiting distinct traits specific to ADPKD. This review described the unique patterns of mineral and bone disorders present in ADPKD in the early CKD stages. The principal points are: the extraosseous FGF23 production by cystic tissues in the kidneys and liver, resulting in elevated circulating FGF23 levels with possible impact on calcium and phosphate balance and cardiovascular risk in ADPKD; the higher prevalence of low bone turnover disease in ADPKD than in other forms of CKD. This is likely due to disruptions in signals mediated by the Polycystin-1 and Polycystin-2 heterodimers, which are expressed on the primary cilia of osteocytes and osteoblasts, leading to impaired bone anabolism. Given these insights, a comprehensive approach is essential for monitoring and managing mineral and bone disorders in ADPKD patients. Early intervention and targeted therapies could mitigate the progression of mineral and bone disorders and possibly improve patient outcomes.
慢性肾脏疾病-常染色体显性遗传性肾脏疾病的矿物质和骨骼紊乱。
常染色体显性多囊肾病(ADPKD)是最常见的遗传性疾病,其特征是双侧肾囊肿从亲代小管分离,逐渐导致肾功能丧失。ADPKD患者代表了慢性肾脏疾病(CKD)个体的一个独特子集,具有共同的CKD特征,同时也表现出ADPKD特有的独特特征。这篇综述描述了早期CKD阶段ADPKD中矿物质和骨骼疾病的独特模式。主要观点是:肾脏和肝脏囊性组织的骨外FGF23产生,导致循环FGF23水平升高,可能影响ADPKD的钙和磷酸盐平衡和心血管风险;低骨转换疾病在ADPKD中的患病率高于其他形式的CKD。这可能是由于polycytin -1和polycytin -2异源二聚体介导的信号中断,这些异源二聚体在骨细胞和成骨细胞的初级纤毛上表达,导致骨合成代谢受损。鉴于这些见解,综合方法对于监测和管理ADPKD患者的矿物质和骨骼疾病至关重要。早期干预和靶向治疗可以缓解矿物质和骨骼疾病的进展,并可能改善患者的预后。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Bone
医学-内分泌学与代谢
CiteScore
8.90
自引率
4.90%
发文量
264
审稿时长
30 days
期刊介绍:
BONE is an interdisciplinary forum for the rapid publication of original articles and reviews on basic, translational, and clinical aspects of bone and mineral metabolism. The Journal also encourages submissions related to interactions of bone with other organ systems, including cartilage, endocrine, muscle, fat, neural, vascular, gastrointestinal, hematopoietic, and immune systems. Particular attention is placed on the application of experimental studies to clinical practice.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


