Clinical evidence linking osteoporosis and the gut microbiome in postmenopausal females: A systematic review
IF 3.6
2区 医学
Q2 ENDOCRINOLOGY & METABOLISM
引用次数: 0
Abstract
Background
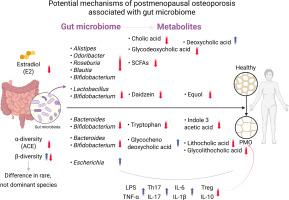
Recent studies have highlighted the intricate relationship between gut microbiome (GM) and osteoporosis (OP), particularly in postmenopausal females. However, the precise mechanisms underlying this association remain unclear.
Materials and methods
This retrospective review and meta-analysis aimed to elucidate the role of GM in postmenopausal OP (PMO) by synthesizing clinical findings from recent literature. A systematic search of four databases (PubMed, Google Scholar, Cochrane Library, and Web of Science) identified 16 relevant clinical studies published between January 2000 and July 2025.
Results
A total of 1520 postmenopausal females (mean age: 59.25 ± 6.63 years) were included, comprising 656 patients with PMO and 864 healthy controls (HC). A meta-analysis of gut microbial α diversity revealed a significant reduction (p = 0.04) in the abundance-based coverage estimator (ACE) index in patients with PMO, indicating a loss of microbial richness. At the same time, β-diversity findings were inconsistent across studies. Taxonomic analysis confirmed differences between patients and HC at the phylum and genus levels. PMO is characterized by a significant increase in primary bile acids and a reduction in tryptophan and daidzein metabolism at the metabolic level. Additionally, Patients with PMO exhibited markedly lower serum estradiol levels, higher levels of lipopolysaccharide and tumor necrosis factor-α, a higher proportion of Th17 cells, and a lower Treg cell population, indicating a pro-inflammatory state.
Conclusion
Overall, this review provides a comprehensive synthesis of current clinical evidence on the role of GM in PMO, emphasizing its potential impact on bone metabolism. Given these findings, targeting the composition of gut microbiota and its metabolites may offer a promising therapeutic strategy for mitigating OP in postmenopausal females.
绝经后女性骨质疏松症与肠道微生物组相关的临床证据:一项系统综述。
背景:最近的研究强调了肠道微生物组(GM)与骨质疏松症(OP)之间的复杂关系,特别是在绝经后女性中。然而,这种关联背后的确切机制尚不清楚。材料和方法:本回顾性研究和荟萃分析旨在通过综合近期文献的临床发现来阐明GM在绝经后OP (PMO)中的作用。对四个数据库(PubMed, b谷歌Scholar, Cochrane Library和Web of Science)进行系统搜索,确定了2000年1月至2025年7月间发表的16项相关临床研究。结果:共纳入绝经后女性1520例(平均年龄59.25 ± 6.63 岁),其中PMO患者656例,健康对照(HC) 864例。一项肠道微生物α多样性的荟萃分析显示,PMO患者的基于丰度的覆盖估计(ACE)指数显著降低(p = 0.04),表明微生物丰富度下降。与此同时,β多样性的发现在不同的研究中并不一致。分类分析证实了患者和HC在门和属水平上的差异。PMO的特点是原发性胆汁酸显著增加,在代谢水平上色氨酸和大豆苷元代谢减少。此外,PMO患者血清雌二醇水平明显降低,脂多糖和肿瘤坏死因子-α水平升高,Th17细胞比例升高,Treg细胞数量减少,表明PMO患者处于促炎状态。结论:总体而言,本文综述了目前关于GM在PMO中的作用的临床证据,强调了其对骨代谢的潜在影响。鉴于这些发现,针对肠道微生物群及其代谢物的组成可能为减轻绝经后女性OP提供了一种有希望的治疗策略。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Bone
医学-内分泌学与代谢
CiteScore
8.90
自引率
4.90%
发文量
264
审稿时长
30 days
期刊介绍:
BONE is an interdisciplinary forum for the rapid publication of original articles and reviews on basic, translational, and clinical aspects of bone and mineral metabolism. The Journal also encourages submissions related to interactions of bone with other organ systems, including cartilage, endocrine, muscle, fat, neural, vascular, gastrointestinal, hematopoietic, and immune systems. Particular attention is placed on the application of experimental studies to clinical practice.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


