Improving nutrition in pediatric heart failure
引用次数: 0
Abstract
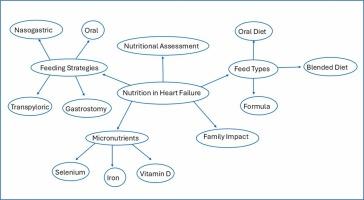
Heart failure occurs in 0.9 to 3 per 100,000 children, and can be the result of either structural heart disease, genetic, or acquired cardiomyopathies. Malnutrition remains a major concern in this population, and results from the complex interplay between decreased dietary intake, decreased absorption, and an altered metabolic state. Assessing nutritional status remains a challenge, with conventional anthropometric measures often being unsuitable. To this end, the Subjective Global Nutrition Assessment has been developed and this, in combination with indirect calorimetry, can be used to give a better estimate of a child’s nutritional status and caloric needs. Determining the best way to meet these needs requires a multidisciplinary team approach, determining both the most appropriate feeding route and most appropriate type of feed. This is particularly important with the trend toward blended feeds, as these feeds must not only meet protein-energy requirements but must also not exceed daily sodium requirements or fluid restrictions. To further optimize heart failure through nutrition, the use of micronutrient supplementation has evolved. In particular, optimizing vitamin D, selenium, and iron has been shown to be beneficial from a heart failure management perspective. As nutrition plays such a vital role in the medical optimization of pediatric patients with heart failure, it is important to acknowledge the impact this can have on the child and the family unit.
改善儿童心力衰竭的营养
每10万名儿童中有0.9至3人发生心力衰竭,可能是结构性心脏病、遗传性或获得性心肌病的结果。营养不良仍然是这一人群的主要问题,这是饮食摄入减少、吸收减少和代谢状态改变之间复杂相互作用的结果。评估营养状况仍然是一个挑战,传统的人体测量方法往往不合适。为此目的,制定了主观全球营养评估,与间接量热法相结合,可以更好地估计儿童的营养状况和热量需求。确定满足这些需求的最佳方法需要一个多学科团队的方法,确定最合适的喂养途径和最合适的饲料类型。在混合饲料的趋势下,这一点尤为重要,因为这些饲料不仅要满足蛋白质能量需求,而且不能超过每日钠需求或液体限制。为了通过营养进一步优化心力衰竭,微量营养素补充剂的使用已经发展。特别是,优化维生素D、硒和铁已被证明从心力衰竭管理的角度是有益的。由于营养在儿科心力衰竭患者的医疗优化中起着至关重要的作用,因此认识到这对儿童和家庭单位的影响是很重要的。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


