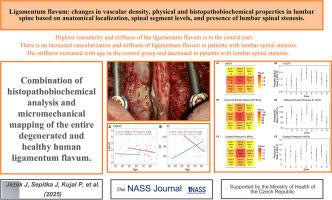
Ligamentum flavum: changes in vascular density, physical and histopathobiochemical properties in lumbar spine based on anatomical localization, spinal segment levels, and presence of lumbar spinal stenosis
IF 2.5
Q3 Medicine
引用次数: 0
Abstract
Background
Hypertrophy of the ligamentum flavum (LF) contributes significantly to the development of lumbar spinal stenosis (LSS), a serious and often disabling disease predominantly affecting the aging population. Histologic changes in the ligament and the tissue mediators that drive these alterations have been described, but their spatial distribution within the ligament remains unclear. Understanding these changes may enable future interventions to slow ligament degeneration and disease progression. To date, no study has comprehensively described the distribution of pathological changes within individual ligaments.
Methods
This study combined histopathobiochemical analysis and micromechanical mapping of healthy and degenerated human LF specimens obtained perioperatively from 57 patients undergoing lumbar spine surgery (38 with LSS and 19 controls). Ligament samples were analyzed histologically for vascular density, presence of inflammatory infiltrates, and chondroid metaplasia using morphometric software and immunohistochemical staining. Mechanical properties, including stiffness (Young’s modulus) and contact pressure, were measured via nanoindentation using the Hysitron BioSoft In-Situ Indenter system. Samples were spatially mapped across 9 anatomical zones of the LF to investigate regional variation. Statistical analyses compared these parameters between spinal segments (L3/4, L4/5, L5/S1), between LSS and control groups, and evaluated age-related trends.
Results
The central region of the LF exhibited significantly higher vascularity and stiffness compared to peripheral regions. Areas showing chondroid metaplasia and inflammation demonstrated increased vascularization, characteristic of LSS pathology. Although vascular density and mechanical stiffness were elevated in LSS patients versus controls, these differences did not reach statistical significance. Age-related trends differed between groups: stiffness increased with age in controls but decreased in LSS patients.
Conclusions
The greatest changes in vascularization and stiffness occur in the central region of ligamentum flavum. Understanding these localized alterations may support future development of targeted therapies to slow or prevent disease progression.
黄韧带:基于解剖定位、脊柱节段水平和腰椎管狭窄存在的腰椎血管密度、物理和组织病理生化特性的变化
背景:黄韧带(LF)肥大是腰椎管狭窄症(LSS)发展的重要因素,这是一种严重且常致残的疾病,主要影响老年人。已经描述了韧带的组织学改变和驱动这些改变的组织介质,但它们在韧带内的空间分布尚不清楚。了解这些变化可能使未来的干预措施能够减缓韧带变性和疾病进展。迄今为止,还没有研究全面描述单个韧带内病理变化的分布。方法对57例腰椎手术患者(38例腰椎失稳组,19例对照组)围手术期获得的健康和退变的人LF标本进行组织病理生化分析和显微力学制图。使用形态测量软件和免疫组织化学染色对韧带样本进行血管密度、炎症浸润和软骨样化生的组织学分析。机械性能,包括刚度(杨氏模量)和接触压力,使用hyysitron BioSoft原位压头系统通过纳米压痕进行测量。样本在空间上绘制了LF的9个解剖区,以研究区域差异。统计学分析比较了LSS组和对照组之间(L3/4、L4/5、L5/S1)、LSS组和对照组之间的这些参数,并评估了年龄相关趋势。结果与外周区域相比,LF的中心区域表现出明显更高的血管密度和僵硬度。显示软骨样化生和炎症的区域显示血管化增加,这是LSS病理的特征。尽管与对照组相比,LSS患者的血管密度和机械刚度升高,但这些差异没有达到统计学意义。与年龄相关的趋势在两组之间有所不同:对照组的僵硬度随着年龄的增长而增加,而LSS患者的僵硬度则随着年龄的增长而下降。结论黄韧带中部的血管化和僵硬程度变化最大。了解这些局部改变可能有助于未来开发靶向治疗,以减缓或预防疾病进展。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

North American Spine Society Journal
Medicine-Surgery
CiteScore
1.80
自引率
0.00%
发文量
71
审稿时长
48 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


