Comparing clinical decision support systems for improving follow-up of abnormal cervical cancer screening test results
IF 4.5
2区 医学
Q2 COMPUTER SCIENCE, INTERDISCIPLINARY APPLICATIONS
引用次数: 0
Abstract
Background
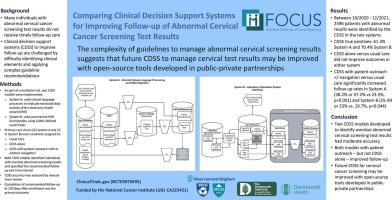
Many individuals with abnormal cervical cancer screening test results do not receive timely follow-up care. Clinical decision support systems (CDSS) to improve follow-up are challenged by difficulty identifying clinical elements and applying complex guideline recommendations. As part of a multisite trial, two CDSS models were implemented: one used natural language processes to evaluate extracted data outside of the electronic health record (EHR) (System A); the other used commercial EHR functionality using LOINC-defined result fields (System B). This secondary analysis compared the accuracy and trial outcomes among sites using these two CDSS models.
Methods
Primary care clinics (32 in System A and 12 in System B) were randomly assigned to usual care, CDSS alone, or CDSS with patient outreach with or without navigation. CDSS identified individuals with overdue abnormal screening results and specified the recommended follow-up and time interval. CDSS accuracy was assessed by manual chart review. Patient outreach consisted of portal/mailed letters plus a single phone call. Navigation included one or more phone calls to address barriers to care. Completion of recommended follow-up at 120 days after enrollment was the primary outcome. Clinic was the unit of randomization, and the patient was the unit of analysis.
Results
Between October 2020 and December 2021, 2596 patients with abnormal results were identified by the CDSS. CDSS true positives were 61.3 % in System A and 70.4 % in System B. CDSS alone versus usual care did not improve outcomes in either system. CDSS with patient outreach with or without navigation versus usual care significantly increased follow-up rates in System A (38.2 % or 37.2 % vs 23.5 %, p < 0.001) and System B (25.4 % or 23 % vs. 19.7 %, p = 0.044).
Conclusions
Two CDSS models developed to identify overdue abnormal cervical cancer screening test results had moderate accuracy. Both models with patient outreach with or without navigation – but not CDSS alone – increased recommended follow-up. Future CDSS for cervical cancer screening may be improved with open-source tools developed in public–private partnerships.
比较临床决策支持系统对改善异常宫颈癌筛查结果随访的作用。
背景:许多宫颈癌筛查结果异常的个体没有得到及时的随访。临床决策支持系统(CDSS),以提高随访困难识别临床因素和应用复杂的指南建议的挑战。作为多站点试验的一部分,实施了两个CDSS模型:一个使用自然语言过程来评估电子健康记录(EHR)(系统a)之外提取的数据;另一个使用商业EHR功能,使用loc定义的结果字段(系统B)。该二次分析比较了使用这两种CDSS模型的站点的准确性和试验结果。方法:初级保健诊所(A系统32家,B系统12家)被随机分配到常规护理、单独CDSS或CDSS患者外展有或没有导航。CDSS对筛查结果逾期异常的个体进行识别,并规定了建议的随访和时间间隔。CDSS的准确性通过人工图表审查来评估。患者外展包括门户/邮寄信件加上一个电话。导航包括一个或多个电话,以解决护理障碍。在入组后120 天完成推荐的随访是主要结局。临床是随机化的单位,病人是分析的单位。结果:在2020年10月至2021年12月期间,CDSS发现了2596例异常结果患者。在A系统中CDSS真阳性为61.3 %,在b系统中为70.4 %。单独使用CDSS与常规护理相比,对两种系统的结果都没有改善。与常规护理相比,有导航或没有导航的CDSS患者外展显著增加了A系统的随访率(38.2 %或37.2 % vs 23.5 %,p )。结论:两种用于识别逾期异常宫颈癌筛查结果的CDSS模型具有中等准确性。这两种模型都增加了推荐的随访,包括有或没有导航的患者外展,而不是单独的CDSS。未来用于子宫颈癌筛查的CDSS可以通过公私合作开发的开源工具得到改进。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Journal of Biomedical Informatics
医学-计算机:跨学科应用
CiteScore
8.90
自引率
6.70%
发文量
243
审稿时长
32 days
期刊介绍:
The Journal of Biomedical Informatics reflects a commitment to high-quality original research papers, reviews, and commentaries in the area of biomedical informatics methodology. Although we publish articles motivated by applications in the biomedical sciences (for example, clinical medicine, health care, population health, and translational bioinformatics), the journal emphasizes reports of new methodologies and techniques that have general applicability and that form the basis for the evolving science of biomedical informatics. Articles on medical devices; evaluations of implemented systems (including clinical trials of information technologies); or papers that provide insight into a biological process, a specific disease, or treatment options would generally be more suitable for publication in other venues. Papers on applications of signal processing and image analysis are often more suitable for biomedical engineering journals or other informatics journals, although we do publish papers that emphasize the information management and knowledge representation/modeling issues that arise in the storage and use of biological signals and images. System descriptions are welcome if they illustrate and substantiate the underlying methodology that is the principal focus of the report and an effort is made to address the generalizability and/or range of application of that methodology. Note also that, given the international nature of JBI, papers that deal with specific languages other than English, or with country-specific health systems or approaches, are acceptable for JBI only if they offer generalizable lessons that are relevant to the broad JBI readership, regardless of their country, language, culture, or health system.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


