Myocardial injury and short- and long-term outcomes after oncological surgery: A large-scale retrospective cohort study
IF 5.1
2区 医学
Q1 ANESTHESIOLOGY
引用次数: 0
Abstract
Background
Myocardial injury after noncardiac surgery (MINS) significantly contributes to perioperative mortality, yet its incidence and prognostic value in patients undergoing oncological surgery remain inadequately characterized.
Methods
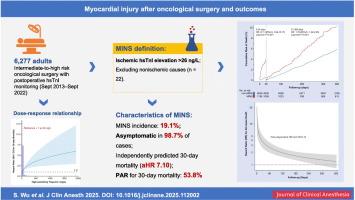
In this retrospective cohort study, we analyzed 6277 adults (mean age 58.9 years; 60.0 % male) undergoing intermediate-to-high-risk oncological surgeries between September 2013 and September 2022 with postoperative high-sensitivity troponin I (hsTnI) measurements. Dose-response relationships between peak hsTnI and the outcomes of 30-day mortality and 30-day major adverse cardiovascular events (MACE) were modeled using multivariable Cox regression with restricted cubic splines. MINS was defined as an ischemic hsTnI elevation >26 ng/L. Long-term (365-day) mortality was analyzed using both 30-day landmark analysis and flexible parametric survival model (FPSM) to account for potential time-varying effects.
Results
Each standard deviation increase in log-transformed hsTnI was associated with a twofold higher risk of 30-day mortality (adjusted hazard ratio [aHR] 2.33, 95 % CI: 1.94–2.80; P < 0.001) and a nearly fourfold higher risk of 30-day MACE (aHR 3.91, 95 % CI: 3.47–4.42; P < 0.001). After excluding 22 patients with nonischemic troponin elevations, MINS occurred in 19.1 % of patients, with 98.7 % being asymptomatic. MINS independently predicted 30-day mortality (aHR 7.10, 95 % CI: 4.21–11.97; P < 0.001) and accounted for 53.8 % of the population-attributable risk. Adding MINS modestly improved the C-index for 30-day mortality prediction (0.831 vs. 0.797; ΔC-index, 0.034; P = 0.090) but significantly improved risk reclassification (net reclassification improvement, 31.51 %) and discrimination (integrated discrimination improvement, 0.037). Landmark analysis showed an 8.1-fold increased risk within 30 days and a sustained 1.8-fold risk from day 31 to 365. FPSM confirmed a sustained excess mortality hazard throughout the year.
Conclusions
MINS is common, largely asymptomatic, and strongly associated with both early and late mortality after oncological surgery. Routine troponin monitoring may help identify high-risk patients for intervention.
肿瘤手术后心肌损伤及短期和长期预后:一项大规模回顾性队列研究
背景:非心脏手术后心肌损伤(MINS)对围手术期死亡率有显著影响,但其在肿瘤手术患者中的发病率和预后价值仍不充分。方法在这项回顾性队列研究中,研究人员分析了2013年9月至2022年9月期间接受中高风险肿瘤手术的6277名成年人(平均年龄58.9岁,60.0%为男性),并测量了术后高灵敏度肌钙蛋白I (hsTnI)。hsTnI峰值与30天死亡率和30天主要不良心血管事件(MACE)结局之间的剂量-反应关系采用限制三次样条多变量Cox回归建模。min定义为缺血性hsTnI升高26 ng/L。使用30天里程碑分析和灵活参数生存模型(FPSM)分析长期(365天)死亡率,以解释潜在的时变效应。结果log-转化hsTnI每增加一个标准差,30天死亡风险增加2倍(校正风险比[aHR] 2.33, 95% CI: 1.94-2.80; P < 0.001), 30天MACE风险增加近4倍(aHR 3.91, 95% CI: 3.47-4.42; P < 0.001)。在排除22例非缺血性肌钙蛋白升高的患者后,19.1%的患者发生MINS,其中98.7%无症状。MINS独立预测30天死亡率(aHR 7.10, 95% CI: 4.21-11.97; P < 0.001),占人口归因风险的53.8%。加入MINS可适度改善30天死亡率预测的c指数(0.831 vs. 0.797; ΔC-index, 0.034; P = 0.090),但可显著改善风险重分类(净重分类改善31.51%)和歧视(综合歧视改善0.037)。里程碑式分析显示,30天内风险增加8.1倍,从31天到365天持续1.8倍的风险。人口普查确认全年存在持续过高的死亡率危险。结论smins是一种常见的、无症状的、与肿瘤手术后早期和晚期死亡率密切相关的疾病。常规肌钙蛋白监测可能有助于识别高危患者进行干预。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
CiteScore
7.40
自引率
4.50%
发文量
346
审稿时长
23 days
期刊介绍:
The Journal of Clinical Anesthesia (JCA) addresses all aspects of anesthesia practice, including anesthetic administration, pharmacokinetics, preoperative and postoperative considerations, coexisting disease and other complicating factors, cost issues, and similar concerns anesthesiologists contend with daily. Exceptionally high standards of presentation and accuracy are maintained.
The core of the journal is original contributions on subjects relevant to clinical practice, and rigorously peer-reviewed. Highly respected international experts have joined together to form the Editorial Board, sharing their years of experience and clinical expertise. Specialized section editors cover the various subspecialties within the field. To keep your practical clinical skills current, the journal bridges the gap between the laboratory and the clinical practice of anesthesiology and critical care to clarify how new insights can improve daily practice.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


