Recto-intercostal fascial plane block: A scoping review
IF 0.7
Q3 ANESTHESIOLOGY
引用次数: 0
Abstract
Background
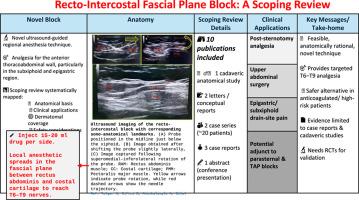
The recto-intercostal fascial plane block (RIFPB) is a novel ultrasound-guided regional anesthesia technique intended to provide analgesia for the anterior thoracoabdominal wall, particularly the subxiphoid and epigastric regions. Unlike established modalities such as thoracic epidural, transversus abdominis plane (TAP) block, or parasternal intercostal plane block (PIPB)—which are limited by side-effect profiles or incomplete cranial/epigastric spread—RIFPB seeks to target intercostal nerves in a safe and relatively avascular plane. Early case reports suggest potential benefits in patients undergoing sternotomy or upper abdominal surgery, but the evidence base remains preliminary.
Objectives
This scoping review aimed to systematically map and synthesize the current evidence on RIFPB, focusing on its anatomical basis, technical feasibility, clinical applications, dermatomal coverage, and safety considerations.
Eligibility criteria
Eligible sources included cadaveric studies, letters, case reports, case series, abstracts, and conceptual reports describing the anatomical spread, technique, or clinical utility of RIFPB. Only studies published in English were considered. Randomized controlled trials were not identified.
Sources of evidence
A comprehensive search was conducted across PubMed, Embase, Scopus, Cochrane Library, and Google Scholar from database inception to June 2025. Grey literature, including professional society proceedings (ASRA, ESRA) and preprint servers (medRxiv, Research Square), was also screened.
Charting methods
Records were imported into EndNote, then transferred to Rayyan.ai for screening. Duplicates were removed manually. Title/abstract and full-text screening were independently performed by two reviewers, with discrepancies resolved by consensus or a third reviewer. A standardized data extraction form (Microsoft Excel) was used to capture study characteristics, technique details, dermatomal coverage, and outcomes.
Results
Ten publications were included: six case reports/letters, one cadaveric study, one conceptual description, one case series, and one conference abstract. Most clinical reports described use in cardiac surgery, typically in combination with a PIPB for sternotomy analgesia. Two reports involved upper abdominal surgery. The cadaveric study demonstrated consistent dye spread between T6–T9, supporting the anatomical rationale for epigastric analgesia. Clinical studies variably reported sensory involvement from T5–T11, although testing methods were inconsistent. No randomized controlled trials were identified. Across available evidence, RIFPB was consistently described as technically feasible, safe, and free from major complications, including in pediatric patients.
Conclusions
RIFPB appears to be a feasible, anatomically rational, and potentially valuable adjunct to the existing repertoire of anterior thoracoabdominal wall blocks. Its ability to provide epigastric analgesia positions it as complementary to PIPB and TAP blocks, particularly in cardiac and upper abdominal surgery. However, the current evidence is limited to preliminary, case-based reports without standardized outcome measures or comparative data. Future research should focus on prospective, randomized trials with validated pain scores, opioid consumption metrics, and safety endpoints to establish efficacy and generalizability. Until then, RIFPB should be regarded as an experimental but promising technique rather than a replacement for established modalities.
直肠-肋间筋膜平面阻滞:范围回顾
背景直肠-肋间筋膜平面阻滞(RIFPB)是一种新型超声引导区域麻醉技术,旨在为前胸腹壁,特别是剑突下和上腹部区域提供镇痛。与诸如胸椎硬膜外阻滞、经腹阻滞或胸骨旁肋间阻滞(PIPB)等已建立的模式不同,这些模式受副作用或颅/腹壁不完全扩张的限制,rifpb寻求在一个安全和相对无血管的平面上靶向肋间神经。早期病例报告表明,接受胸骨切开术或上腹部手术的患者可能受益,但证据基础仍处于初步阶段。本综述旨在系统地绘制和综合目前关于RIFPB的证据,重点关注其解剖学基础、技术可行性、临床应用、皮肤覆盖范围和安全性考虑。合格来源包括尸体研究、信件、病例报告、病例系列、摘要和描述RIFPB解剖分布、技术或临床应用的概念性报告。只考虑了用英语发表的研究。没有确定随机对照试验。证据来源从数据库建立到2025年6月,对PubMed、Embase、Scopus、Cochrane Library和b谷歌Scholar进行了全面检索。灰色文献,包括专业学会会刊(ASRA, ESRA)和预印本服务器(medRxiv, Research Square)也被筛选。绘制图表的方法记录被导入到EndNote,然后转移到Rayyan。我要筛选。已手动删除重复项。标题/摘要和全文筛选由两位审稿人独立完成,差异由共识或第三方审稿人解决。使用标准化数据提取表(Microsoft Excel)捕获研究特征、技术细节、皮肤覆盖和结果。结果共收录文献6篇:病例报告/信函1篇,尸体研究1篇,概念描述1篇,病例系列1篇,会议摘要1篇。大多数临床报告描述了在心脏手术中使用,通常与PIPB联合用于胸骨切开镇痛。两份报告涉及上腹部手术。尸体研究表明T6-T9之间的染色分布一致,支持上腹部镇痛的解剖学原理。尽管测试方法不一致,但临床研究报告T5-T11的感觉受累情况不一。未发现随机对照试验。在现有的证据中,RIFPB一直被描述为技术上可行、安全、无主要并发症,包括在儿科患者中。结论rifpb似乎是一种可行的、解剖学上合理的、潜在的有价值的前胸腹壁阻滞的辅助手段。其提供上腹部镇痛的能力使其成为PIPB和TAP阻滞的补充,特别是在心脏和上腹部手术中。然而,目前的证据仅限于初步的基于病例的报告,没有标准化的结果测量或比较数据。未来的研究应侧重于前瞻性、随机试验,包括经过验证的疼痛评分、阿片类药物消耗指标和安全终点,以确定疗效和普遍性。在此之前,RIFPB应被视为一种实验性但有前途的技术,而不是替代现有模式。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Trends in Anaesthesia and Critical Care
ANESTHESIOLOGY-
CiteScore
1.90
自引率
13.30%
发文量
60
审稿时长
33 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


