The efficacy of thoracic duct ligation for post-esophagectomy chylothorax in esophageal cancer: a nationwide inpatient cohort study
IF 2.4
4区 医学
Q3 ONCOLOGY
引用次数: 0
Abstract
Background
Recently, thoracic duct embolization (TDE) has been increasingly adopted as a first-line minimally invasive therapy for post-esophagectomy chylothorax instead of thoracoscopic thoracic duct ligation (TTDL). However, the therapeutic efficacy and advantages of TDE over TTDL are still controversial. This study aimed to evaluate and compare the clinical and financial outcomes of TDE and TTDL for post-operative chylothorax after esophagectomy using a national database.
Methods
We retrieved data from patients with esophageal cancer who underwent TDE (n = 312) or TTDL (n = 167) for chylothorax after esophagectomy between April 2012 and March 2022 from the Diagnosis Procedure Combination database in Japan. We compared the success rate of the first intervention, length of post-interventional hospital stay, and total hospitalization cost between the TDE and TTDL groups using propensity score matching analysis.
Results
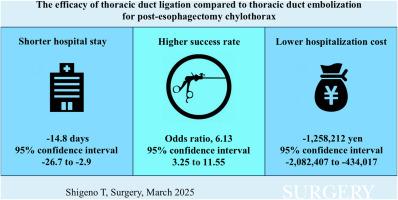
The success rate of the first intervention was significantly higher in the TTDL group than in the TDE group (odds ratio, 6.13; 95 % confidence interval [CI], 3.25 to 11.55). The length of post-interventional hospital stay was significantly shorter (regression coefficient, −14.8 days; 95 % CI, −26.7 to −2.9) and the total hospitalization cost was significantly lower in the TTDL group than in the TDE group (regression coefficient, −1,258,212 yen; 95 % CI, −2,082,407 to −434,017).
Conclusions
This nationwide cohort study showed that TTDL was associated with a shorter length of post-interventional hospital stay, lower total hospitalization cost, and higher success rate of the first intervention than TDE for post-esophagectomy chylothorax.
食管癌食管切除术后乳糜胸行胸导管结扎治疗的疗效:一项全国住院患者队列研究
近年来,胸导管栓塞术(TDE)已逐渐取代胸腔镜下的胸导管结扎术(TTDL),成为食管切除术后乳糜胸的一线微创治疗方法。然而,TDE相对于TTDL的治疗效果和优势仍存在争议。本研究旨在利用国家数据库评估和比较TDE和TTDL治疗食管切除术后乳糜胸的临床和财务结果。方法我们从日本的诊断程序组合数据库中检索2012年4月至2022年3月期间食管癌食管切除术后乳糜胸行TDE (n = 312)或TTDL (n = 167)的患者数据。我们使用倾向评分匹配分析比较了TDE组和TTDL组的首次干预成功率、介入后住院时间和总住院费用。结果TTDL组首次干预成功率显著高于TDE组(优势比为6.13;95%可信区间[CI], 3.25 ~ 11.55)。TTDL组介入后住院时间显著短于TDE组(回归系数为- 14.8天,95% CI为- 26.7 ~ - 2.9),总住院费用显著低于TDE组(回归系数为- 1,258,212日元,95% CI为- 2,082,407 ~ - 434,017)。结论:这项全国性队列研究表明,与TDE相比,TTDL治疗食管切除术后乳糜胸的介入后住院时间更短,总住院费用更低,首次干预成功率更高。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Surgical Oncology-Oxford
医学-外科
CiteScore
4.50
自引率
0.00%
发文量
169
审稿时长
38 days
期刊介绍:
Surgical Oncology is a peer reviewed journal publishing review articles that contribute to the advancement of knowledge in surgical oncology and related fields of interest. Articles represent a spectrum of current technology in oncology research as well as those concerning clinical trials, surgical technique, methods of investigation and patient evaluation. Surgical Oncology publishes comprehensive Reviews that examine individual topics in considerable detail, in addition to editorials and commentaries which focus on selected papers. The journal also publishes special issues which explore topics of interest to surgical oncologists in great detail - outlining recent advancements and providing readers with the most up to date information.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


