Developing and implementing an obesity medicine fellowship program: Experience at a U.S. academic medical center
引用次数: 0
Abstract
Background
Obesity is a prevalent and complex chronic disease yet physicians’ training in obesity care is often inadequate. Fellowship training in obesity medicine is now available at multiple academic medical centers; however, there has been limited description and evaluation of these programs to date. Therefore, this article describes our curriculum development process and fellowship program implementation experience at a U.S. academic medical center.
Methods
This was a structured, multi-phase curriculum development study guided by established obesity medicine competencies and certification standards. We used a six-step approach to curriculum development to guide our design with content informed by the Obesity Medicine Education Collaborative competencies, American Board of Obesity Medicine (ABOM) content outline, and Accreditation Council for Graduate Medical Education - International Obesity Medicine Fellowship program requirements. We utilized several tools of instruction as well as modes of assessing learners. Feedback from fellows and faculty was used to iteratively refine the program over the initial 3 years.
Results
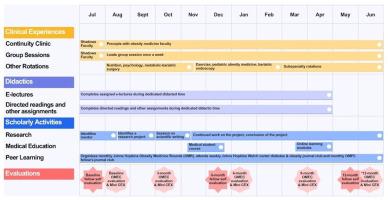
We identified 19 content domains key for obesity medicine. Within each domain, we created instructional components including didactic e-lectures, directed readings, reflective assignments, role play activities, and clinical experiences. We developed evaluation tools to determine trainee progress including knowledge check assessments, mini-clinical evaluation exercises (mini-CEXs), and structured feedback. Early outcomes indicate that trainees achieve competence in obesity care, engage in meaningful scholarly activity, and benefit from professional development opportunities. All graduating fellows have successfully achieved ABOM certification. Feedback has informed fellowship refinements, particularly improvements in rotation timing and duration as well as additional subspecialty elective options.
Conclusion
This obesity medicine fellowship curriculum provides a structured, multidisciplinary program and graduates have achieved competency in obesity care. Obesity medicine fellowship training holds promise in advancing the field through innovative education and leadership development.
发展和实施肥胖医学奖学金计划:在美国学术医疗中心的经验
背景:肥胖是一种普遍而复杂的慢性疾病,但医生在肥胖护理方面的培训往往不足。肥胖医学的奖学金培训现在在多个学术医疗中心提供;然而,迄今为止,对这些项目的描述和评估都很有限。因此,本文描述了我们在美国学术医疗中心的课程开发过程和奖学金项目的实施经验。方法本研究是一项结构化的、多阶段的课程开发研究,以既定的肥胖医学能力和认证标准为指导。我们采用六步法来指导课程设计,内容参考肥胖医学教育合作能力、美国肥胖医学委员会(ABOM)内容大纲和研究生医学教育认证委员会-国际肥胖医学奖学金项目要求。我们使用了几种教学工具以及评估学习者的模式。在最初的3年里,研究员和教师的反馈被用来迭代地完善这个项目。结果鉴定出19个肥胖医学关键内容域。在每个领域中,我们创建了教学组件,包括教学电子讲座、指导阅读、反思作业、角色扮演活动和临床经验。我们开发了评估工具来确定受训人员的进步,包括知识检查评估、迷你临床评估练习(mini- ces)和结构化反馈。早期结果表明,受训者在肥胖护理方面获得了能力,参与了有意义的学术活动,并从专业发展机会中受益。所有毕业生均成功取得ABOM认证。反馈已经告知奖学金的改进,特别是轮转时间和持续时间的改进,以及额外的亚专业选修选项。结论该肥胖医学奖学金课程提供了一个结构化的、多学科的课程,毕业生已具备肥胖护理的能力。肥胖医学奖学金培训有望通过创新教育和领导力发展推动该领域的发展。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


